This post copies a letter sent to Michelle O’Neill and Jeffrey Donaldson, the leaders of the two largest parties in Northern Ireland. It was sent with the letters to Eluned Morgan in Wales and Johnny Mercer in England featured here and on RxISK last week.
The image is of Newgrange on the shortest day of the year – thought to be one of the most magical and hopeful symbols in Ireland. Newgrange is right beside the Boyne River a symbol of Ireland’s deepest divisions. Some references have links not in the original letter.
Michelle O’Neill MLA Jeffrey Donaldson MP
Coalisland Sinn Fein Office The Old Town Hall
Coalisland Lisburn
Co Tyrone BT71 4LN Co Antrim BT27 4DH
August 15 2021
Dear Michelle O’Neill and Jeffrey Donaldson
Let me mention before proceeding that I briefly met Ms. O’Neill on Zoom a year ago, prior to a single meeting with members of Sinn Fein instigated by me hoping to alert them to health policy issues stemming from a 2019 inquest on Stephen O’Neill, an in-law of Ms. O’Neill’s.
I had been approached over a year prior to the inquest by Colleen Bell to offer expert input. I had no idea of Stephen’s background. Bell and O’Neill are surnames from both sides of the political divide. I would have agreed to help regardless of background in this case.
The inquest pointed to significant healthcare issues that affect all of the Western World, are getting worse, and may underpin some of the political divisions we now see linked to Covid.
My post-inquest meeting with Sinn Fein was aimed at drawing out the economic implications of issues such as the ghostwriting of the medical literature and lack of access to clinical trial data that are also leading to deaths like Stephen’s. Just so you and other readers are clear on what ghostwriting means – the academic names, even from the most distinguished institutions, on the authorship lines of medical articles about current drug treatments appearing in the most prestigious journals will not have written those articles or ever have seen the data underpinning them. The ghosts will not have seen the data either.
The NHS hinges on an assumption that effective treatments that save lives and get people back to work will pay for themselves. It cannot survive if flooded with treatments that cost lives and disable people – treatments typified by the sertraline that triggered Stephen’s problems. (See Morgan vs Morgan: The Future of the NHS).
Your ability to bargain on the price of drugs hinges on pharma being able to claim the latest drug works fabulously and is free of risks. Access to trial data levels this playing field.
Given that Sinn Fein had no prior involvement in setting up the features of the system now causing problems, they seemed less likely to be hamstrung by their past. It doesn’t, however, take much exposure to the system to become an insider.
Sinn Fein’s roots in the Irish Co-operative Movement offered a further reason to hope they might engage. The issues linked to Stephen’s death are neither Right nor Left issues. They need politicians and activists to chart a path between Right and Left, as the co-operative movement once did, and AIDS activists did in the 1980s and 1990s.
Having made these points, my sense is that the DUP might have more libertarian leanings than Sinn Fein who perhaps are more authoritarian, and these leanings may play a greater part than anything else in how either of you receive this letter.
When my contact with Sinn Fein came to nothing, I reached out to Green parties also trying to chart a path between Right and Left, but whose health policies depend on technologies, which, no matter how innovative, seem at odds with their environmental policies.
This outreach led to a Politics of Care Forum, where my concerns are laid out. Two posts there – Can Politicians Save Us? and Can Politicians Save the World? – convey key points.
The Crack of Doom forum post has my correspondence with NICE, MHRA, the four Depts. of Health in the UK, the BMA, Brenda Hale and others, linked to Stephen’s inquest. The only missing document is a May 2020 letter from Gillian Leng, the new CEO of NICE, to Ms. O’Neill. This letter confirms what I’ve been saying about NICE Guidelines being based on a ghost-written literature. Ms. Leng’s points about good practices are designed to distract.
Don’t let the silence surrounding the ghost writing of the medical literature and lack of access to trial data mislead you. Western Life Expectancies have been falling prior to Covid. A polypharmacy promoted by a ghostwritten literature that hypes the benefits and hides the harms, with no-one able to check the claims being made, plays a part in this. We are also not meeting population replacement rates owing in part for the same reasons, and specifically to drugs like those Stephen was prescribed.
The silence means that problems about ghostwriting, building guidelines based on a ghostwritten literature, and the sequestration of trial data, are more embarrassing and awkward to those in a position to make a difference than the deteriorating global climate.
When it comes to climate change, nobody thinks swapping our car for a bicycle will make much difference. When it comes to the deteriorating climate in healthcare, many talk about reversing corporate influence but as with climate change no citizens can see a way to do this. My personal view is that it is doctors more than companies who are letting us down.
Healthcare, however, does offer a way for individuals to make a difference – standing our ground on treatment related adverse events.
Hold Your Own Inquest
The possibilities become clear if you consider inquests. Getting out the far side of one is more difficult than getting out of a Maze. Like cricket perhaps, the wider inquest system as it stands embodies an English idea of Fair-Play – eleven against one. Bereaved families would be better advised to hold their own inquests.
Statutory inquests mean:
- Pitting decades worth of knowledge a family has of someone against a 10-minute slot a doctor has given him or her, and having your knowledge dismissed.
- Pitting the possible bias of a family unwilling to think the worst of a child, or parent, against the undoubted bias of a doctor unwilling to contemplate their role in killing someone. The family ends up viewed as too biased to be believable.
- Pitting an Evident transformation in someone seen by many people against Evidence consisting of a ghostwritten literature denying these transformations can happen – with no-one able to check this out, not you, nor any prescribers, nor MHRA. At inquest, the ‘Evidence’ counts for more than what is screamingly Evident.
- Pitting a common-sense causality, that comes close to what the Federal Judicial Manuals in the US mandate as the way to establish causality in drug induced injury, an approach that doctors once took, and losing out to the view of a prescriber who today has no training in determining drug induced causality and is swamped by ‘Evidence’ telling him to avoid common sense.
- Pitting what the company view in private might be against what they say in public about you and your family (see Healy to Morgan).
If you want to make the Statutory System work properly and advance public health:
- You would have to enable coroners to finger a prescription drug as the obvious cause of a death, the way they can with a street drug.
- You would have to work out a way to stop medical insurers blocking doctors like Dr Brannigan in the O’Neill inquest or Dr Adams in the Morgan inquest (Appendix 1), admitting a drug caused a problem.
- You would have to provide guidance to inquest hearings that a ghostwritten literature with no access to trial data is not evidence that can be relied upon.
- You would need to review the evidence admissible at inquests. In the O’Neill inquest, the coroner mistakenly refused to admit evidence from FDA reports of harms on the medicines Stephen was given. Regulators strip names off these reports making them hearsay, but the analysis presented to O’Neill inquest wasn’t hearsay.
You can overcome the coroner’s confusion in the O’Neill case by encouraging doctors and patients to submit reports to companies (rather than regulators) with both doctor and patient names attached so that these are no longer hearsay but more reliable evidence than the current company trial evidence. (See Can Doctors Save Us). Ideally these reports is would also be lodged in a setting that can be accessed in the event of inquests and legal cases so that doctors and patients can be called as witnesses. At present there is no point in doctors or patients reporting to MHRA.
- You would need to educate coroners on the futility of sending regulation 28 reports to MHRA. Unless the regulator changes their spots, they have no role to play in public health other than their current role which is to regulate the wording of adverts. They don’t even regulate the claims made in the adverts parading as medical articles, which are ghostwritten and optimized to sell drugs rather than promote safety.
- You would need to make clear that MHRA responses telling coroners and politicians, that in addition to warnings they depend on the clinical judgment of doctors, avails of the notion of a doctor as a Learned Intermediary. This notion made sense until 1990. Since then, medical learning about drugs and devices comes from a ghostwritten literature with no chance to check the claims against the data. It is no longer clear that doctor’s judgments are worth any more than salt that has lost its saltiness.
- You would need to ensure doctors, and increasingly nurses and others who prescribe, have training in how to establish whether a treatment is causing a problem – none have any training in this basic skill at present.
As things stand every family who has a member whose death is linked to treatment in healthcare would be better off holding their own inquest rather than trying to escape a Maze, where everybody you might refer them to – NICE, MHRA, BMA, Legal Authorities – will whisper their agreement there is a problem but will say it’s not theirs to remedy.
As a woman who lost her 15-year-old daughter to a prescription drug said to June Raine of MHRA:
It would have been better if she had been murdered – that way I could face the perpetrator in court.
Beyond Inquests
The problems come to a dramatic head at an inquest. The same problems hold true for all adverse events on a drug. At least at inquests, if they are damming the dead with the deceased’s family present, doctors express sympathy. Raise an adverse event in their office where no-one can see them and you will often face frank hostility or ridicule.
Still there are possibilities for significant change, which you may sense from Tracey, whose story was recently posted on RxISK.org – What’s a Life Worth?
Tracey’s MP is Johnny Mercer whose resignation as a matter of honour a year ago had an effect in Northern Ireland. I’ve challenged him to pick up these issues – see Appendix 2. As a matter of honour, tolerating deceit, indeed proven fraud, on the scale we now have without calling it out is surely not an option.
The Conservatives, like the Republicans in the US, seem to have turned to populism. This is not a bad thing. The treatment induced problems affecting Mr Mercer’s constituents offer a basis for populism 101, pitting forgotten men and women like Stephen and Tracey against an unthinking bureaucratic system.
I have also written to Eluned Morgan, the Welsh Labour Minister for Health, in response to the inadequate way the system, she has responsibility for, has operated in the wake of the death of Samuel Morgan, killed by an SSRI drug like Stephen (Appendix 1).
Labour in Britain and the Democrats in the US may be the biggest obstacle to the changes needed. They are still campaigning for access to drugs, not realising this is a primrose path to polypharmacy. They, and you, should be campaigning for the information that transforms chemicals into medicines, the absence of which is rapidly making prescription chemicals more dangerous that street chemicals.
With street chemicals our natural caution comes into play, no-one is going to tell us the drug didn’t harm us when we are injured, and coroners can register a street drug as a cause of death but cannot do the same for a prescription drug.
There is a wrinkle though in my hopes for action from Mr. Mercer. Women most often get put on and harmed by these drugs, but Army recruits and veterans are another badly affected group. The British Establishment has denied the risks to its troops from medical treatments, as vehemently as Mr. Mercer stone-walled Tracey. How far will his sense of duty to veterans take him?
The denial of risks starts with doxycycline, which may have initiated Stephen’s problems, followed by mefloquine (Lariam). These are used when troops are deployed to areas where malaria is common. Both commonly cause suicide – as in the horrific death of 19-year-old Amanda Cutland that featured on the front pages of most British newspapers 2 years ago. The coroner was shocked, but MHRA took the opportunity to hone their skills at denying the undeniable. (I can send you details).
Then there is sertraline, which made Stephen’s problems worse. This is dished out to Army veterans for PTSD. Neither the veterans getting it, nor the doctors dishing it out, will know that prior to its licensing for PTSD all four of the trials done were negative for men. There was a flicker of benefit for women in two of these trials – women who did not have the kind of condition soldiers have.
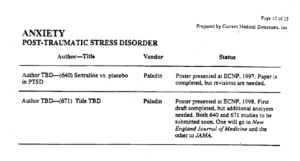
A previously senior FDA figure, Paul Leber, was drafted in by Pfizer to help get sertraline approved by FDA for PTSD, despite it not meeting criteria for approval. Its licensing for PTSD gave rise to a prize exhibit in my argument that the clinical trial literature is now ghost written and there is no access to trial data.
In the slide below from 1999, TBD means To Be Determined. The articles had already been written by ghosts. The Pfizer marketing department at this point needed to decide whose names, featured as authors, would sell the most sertraline (Zoloft).
Politicians
In raising these issues, one or both of you could do more to reduce deaths among British Army personnel than were ever linked to the Troubles and reduce the number of homicides of innocent civilians, of which at present there are likely a greater number triggered by SSRIs every year or so among Army personnel or veterans than might have happened at the hands of the Army in Northern Ireland.
It is the best and worst of times to raise these issues. No-one wants to shake confidence in the vaccine program.
The system, however, that enables Pfizer bring a pretty ineffective drug like sertraline on the market without scrutiny of the underlying data, and can let them ghost write out of existence hazards like sertraline induced suicides and homicides, triggered both by starting it and stopping it, is the system through which we now bring vaccines to market. Nothing has changed. If anything, we have a Maze that is more difficult to escape.
Many people are clearly conflicted. Their difficulties are characterized as stemming from ignorance rather than a sense that something is amiss, even though surveys that have nothing to do with vaccines show a waning of public trust in drug regulators and the bodies representing medical professionals.
There is a lot that is amiss. The greatest concentration of fake literature on earth centres on the medicines doctors give you and your family and friends.
Two decades ago, when I became aware of the problems outlined here, I contacted MHRA suggesting I should not be saying things as serious as this if they are wrong. I offered to meet them and stop saying what I was saying if persuaded of the error of my ways. We met. They didn’t contest a single point. Soon after, a crisis blew up about these drugs that led to Black Box Warnings, and billion-dollar fines, but not the changes the crisis called for.
At a House of Commons Select Committee in mid-crisis, I repeated the points on the record, while figures like Iain Chalmers of the Cochrane Collaboration and Richard Horton, editor of the Lancet, downplayed concerns without attempting to rebut them. Neither Cochrane nor the Lancet look particularly good now.
I repeat my MHRA offer. I am happy to engage with anyone you suggest might point out the mistakes in what I am saying. If no-one is willing to engage in public on these issues, and over twenty years no-one has, I think the onus is on one of you to take a lead within the United Kingdom and the European Community not on chemicals that have to cross borders but on information critical to the safety of your constituents that should be universal.
While not without risks, this is a time when a politician who can seize the moment could exert significant leverage. Whatever about Reconciliation, a Truth Commission is called for. If either of you rises to the moment, I would be happy to help regardless of political background.
Yours sincerely
David Healy MD FRCPsych
See Can Politicians Save Us and Can Politicians Save the World

When will it ever end.
Aug 9, 2021, 8:49 PM
to curricula consultation (re David Healy blogs )
FAO John Russell Associate Dean
Regarding the above can you tell me if there re any plans to include the issues highlighted in discussions about the curricula ?
Thank you (encl blogs)
Susanne
Dear ‘Molly’
FAO John Russell Associate Dean
Thank you for your reply of Aug.13 2021
Can you kindly forward the above written by Professor David Healy as additional feedback to the Curricula consultation .Susanne
Also
Date: Mon, Aug 9, 2021 at 7:25 P
to Adrian James
https://rxisk.org/whats-a-life-worth-is-anyone-listening/#comments
FAO The President (re copy of Tracey’s account)
There are many accounts being published by those who have been damaged by their experience of psychiatry and prescribed drugs. They are so often undermined -but when so many reliable accounts are circulating – can you advise how people who are debating or already accessing services – can trust they will not experience the same damage which as you know has serious very consequences .
Thank you I would appreciate a response which I could circulate to clarify how the college aims to tackle the issue highlighted which is of serious concern.
Susanne
Adrian James
Fri, Aug 13, 4:46 PM (10 days ago)
Dear Susanne
I hope you are well.
Thank you for writing to me.
Whilst the College is not responsible for developing clinical guidelines or regulating psychiatrists, which are the responsibilities of the National Institute for Health and Clinical Excellence (NICE) and General Medical Council (GMC) respectively, we do aim to promote the high standards of care. You specifically mentioned prescribed drugs in your enquiry, which is an area the College has shown leadership. For example, in 2019, we published a position statement stressing the importance of only prescribing antidepressants when clinically indicated, and supporting a much greater focus on safely managing withdrawal. On the latter, we subsequently published a patient information resource on ‘Stopping antidepressants’ to provide general advice on the symptoms that can occur as a result, and ways to reduce and avoid these. These documents have been widely publicised by the College, and we continue to engage with stakeholders about all of these areas to ensure patients have access to all evidence-based treatment options.
All the best,
Adrian
Dear Adrian
Likewise I hope you are well.
Thank you for responding . I will circulate your letter as the message is not getting to everyone yet – neither prescribers or those who consult doctors and other health workers.
I hope this will speed things up Susanne
Sun, Aug 15, 9:17 PM (8 days ago)
Dear Adrian
Thank you for your letter and the documents enclosed. But we need to get to the heart of the matter. The practice as well as the reputation of psychiatry is being damaged as more negative publicity circulates . And to be honest I believe the skills of psychiatrists to relate and help another are being lost by the expectation that it is imperative to follow guidelines without access to the data which informs them. These are flawed by the data not being made available even when drawing up these guidelines.
The College is aware that people are still being harmed and dying from prescribed drugs , much could be avoided in prescribers had better knowlege and guidance, not just guidelines ,to draw on. They are being told to rely on NICE; MHRA neither of whom have access to actual pharmaceutical data themselves . What is published including in journals which people access for information is ghost written, something most would find an unreliable source if it became widely known.
Most people have no real choice but to rely on the information conveyed by doctors. People do reasonably assume that the College is responsible for having actual information from pharmaceutical companies before advising on drug prescribing.
This is the nub of the problem. Nobody is taking responsibility to tackle the problem, whether NICE; MHRA; GMC or when a suicide is considered an effect of prescribed drugs, Coroners seem unable to document this on a death certificate.
Finally, it is a frightening situation whereby those who practice and regulate are leaving known loopholes which can lead to lifelong harms and deaths.
Is the college doing anything to gain the right to access data from pharmaceutical companies and prevent the use of ghost writers which are of course informing how people will be influenced and use prescribed drugs ? Without this Drs cannot treat with confidence of ‘doing no harm’ and those who consult them cannot give informed consent .
With best wishes
Susanne
I have sent this reply pointing out that none of this or the information contained in his letter or documents contained addresses the issues detailed by Davd H, and also written to to the Dean separately -who is heading updates to the Curricula, which will be fed into the GMC.
From: Susanne
Sent: 18 August 2021 11:33
To: Curricula
Subject: Re: dav – Morgan vs Morgan: The Future of the NHS? | Dr. David HealyRE: dav – Morgan vs Morgan: The Future of the NHS? | Dr. David Healy
david healy
Curricula
Wed, Aug 18, 4:00 PM (5 days ago)
to me
Hi Susanne,
Feedback from the consultation will be fed into our final submission to the GMC on the 3rd September.
We will be in contact after that date to explain how we incorporated it into the curricula.
Best,
Molly
Interview: Researchers Deconstruct Ghostwritten Industry Trial for Antidepressant
By Justin Karter
May 14, 2016
https://www.madinamerica.com/2016/05/researchers-deconstruct-ghostwritten-industry-trial-for-antidepressant/
The same thing has been going on with the SSRIs and, in particular, when you’re dealing with a very vulnerable patient population such as children and adolescents, you have a real problem concerning trust in the medical literature. This is not only an issue for prescribing doctors, but it is also a problem for people who set health care policy in government. Also, these articles are very often used in court when the pharmaceutical companies try to defend themselves. So, not only do you have fraud on the medical community but you also have potential fraud in the courts.
So, how can you possibly claim to have evidence-based practice if it turns out that what you are relying upon is medical journals that are publishing ghostwritten misrepresented results from clinical trials? The vast majority of studies published are industry-funded studies. You have a serious problem here for evidence-based medicine.
What’s in a Name? Ghostly Spirits, Spinning Science to Sell Drugs, Stalk the Medical Literature
By Myron Levin
on November 6, 2019
https://www.fairwarning.org/2019/11/whats-in-a-name-ghost-writing-in-medical-literature/
One planned paper on a Paxil clinical trial was shelved because ”the side effect data analysis was terribly unfavorable to our favorite antidepressant. And we hate when that happens,” quipped a Dec. 14, 2000 email from Scientific Therapeutics. “There are some data that no amount of spin will fix,” another email said.
At odds with the data
But soon after, a paper about another clinical trial, called Study 329, triggered a wave of off-label prescribing of Paxil for adolescent depression. The article, published in the Journal of the American Academy of Child and Adolescent Psychiatry, concluded that Paxil “is generally well tolerated and effective for major depression in adolescents.” It would later be attacked as an extreme example of spin and distortion. It ”was largely ghostwritten,” according to a 2015 article in The BMJ, and ”claimed efficacy and safety … that was at odds with the data.”
The manuscript was drafted by Sally K. Laden of Scientific Therapeutics, who had also penned the email about ”our favorite antidepressant.” The lead author, Dr. Martin B. Keller, thanked Laden in a letter. “You did a superb job with this,” he wrote, adding that he and two co-authors were sending some ”rather minor changes.” Published in July, 2001, the article listed 22 authors, but not Laden. A footnote stated: “Editorial assistance was provided by Sally K. Laden, M.S. ”
FairWarning…
We will be providing hope for those whom the status quo is not working by combining the proven therapeutic potential of ketamine with psychotherapy to treat Addiction, Anxiety, Depression, PTSD, and Eating Disorders.
At Awakn Clinics, our clients will be placed at the centre of their care plans. Flexibility will be key. We see our clients as individuals, with their own difficulties and needs. We will offer a true alternative to antidepressants, which is bespoke and collaboratively formulated between client and therapist. is a street drug.
AWAKN – get it? Ketamine is a party drug and also used as hallucinagenic consciousness raising drug – like LSD which is another drug David Knutt has has developed privately to make alcohol free drinks A class of drugs Aldous Huxley described in Heaven and Hell = no telling which a person will potentially experience after taking them
People can be convicted of an offence if caught using or selling it. They are at risk of severe side effects including suicidal thoughts and death. Coroners are able to put drug related death on inquest reports and certificates when the drug has been used recreationally.Why is it not an offence to use it in private ketamine clinics such as set up by David Knutt and colleagues in Bristol when the risks of adverse effects is presumably the same. And why if a person dies as a result of ketamine being prescribed ,should that not be recorded equally as drug related..
A 12 treatment will cost £6000 Not sure what the cost at a rave would be.
Interesting ‘Notice Regarding Forward-Looking Information ‘
on Awakn website. They are being very cautious about the future, probably written more for their protection re potential investors – although I know zilch about his kind of thing.
1 of 1
Re: Suicide and precribed drugs
Awakn Life Sciences
6:56 PM (2 hours ago)
to me
Dear Susanne,
Thank you for expressing an interest in our treatment and clinical trials, however we regret to inform you that we are not conducting any clinical trials at present or in the near future.
Kind regards, (Anthony Tennyson CEO)
E: info@awaknlifesciences.com
On Wednesday, 25 August 2021, 19:13:05 +0100,
Dear Anthony Tennyson
Thank you for your letter and information about what Awakn has achieved already re trials and treatments.
When I read this I was impressed that you are thinking outside the box so thought I would ask if you are doing any work on treating people with prescribed drug induced suicidal thoughts and other adverse effects from especially but not only psychiatric medications.
You will know that there is nowadays advice about this from regulators and on information leafletts and so on – but there is no treatment available to those who do suffer adverse effects of medications.
Individuals are commonly told their symptoms are caused by their illness and prescribed yet more drugs.
If a group such as Awakn which is thinking outside the box could get involved – it would give hope to those for whom no real help otherwise is being undertaken
I am sure there would be many individuals who to be honest feel abandoned and hopeless who would be interested in volunteering to participate in research with Awakn.
Hope to hear from as to what you think?
With best wishes
Susanne
A Good Bag of Nutts, but even better are these Pistachios…
Simon Wessely Retweeted
Richard Vautrey
@rvautrey
·
26 Aug
My letter to Daily Telegraph published today in response to unacceptable and demoralising article on GP appointments. The hard work of GPs and their teams should be celebrated not condemned. Join our @BMA_GP #supportyoursurgery campaign.
https://www.bma.org.uk/bma-media-centre/bma-letter-to-daily-telegraph-in-response-to-article-on-gp-appointments
Clare Gerada
@ClareGerada
·
26 Aug
gp-crisis-serious-covid-doctor-state-profession-day-in-life> thanks
@RachelPugh2
for being the first Journaliat to actually spend time with me in my GP role in > 30 years and see what we do that is unseen by everyone else.
https://inews.co.uk/news/long-reads/gp-crisis-is-as-serious-an-issue-as-covid-a-doctor-on-why-she-is-furious-about-the-state-of-her-profession-1167646
GPs are improving their work-life balance while worsening the life-death balance of everyone else
Distress at being unable to see a doctor in person has hardened into cynicism – it’s no wonder long-suffering patients are losing it
https://www.telegraph.co.uk/columnists/2021/08/24/gps-improving-work-life-balance-worsening-life-death-balan
Prof David Healy writes that the RCPsych has in fact known about the problem with antidepressant withdrawal for many years. He writes:
“Successive presidents of the British Psychiatric College have been told about this problem for over 20 years since Charles Medawar first wrote to them. They are in great part personally responsible for ongoing injuries from disbelief to thousands, maybe hundreds of thousands of people.”
He suggests it is time for Prof Wendy Burn, current President, and Prof Simon Wessely, former President and husband of Prof Clare Gerada, to “man up”.
https://davidhealy.org/the-horrific-effects-of-not-being-believed/
Anyone who is complicit in maintaining this silence, is also complicit in causing immense suffering to patients and for standing by and doing absolutely nothing about it. I believe this should now be a criminal matter.
Powerful Embrace
https://vimeo.com/101303835
One of the best lines of Comments – EVER
The His and Her Guide to Holidaying in Scotland…
https://nevertrustadoctor.wordpress.com/2018/04/23/silence-like-a-cancer-grows-the-shocking-truth-about-antidepressants/
Crisis in General Practice. Silence like a cancer grows.
The NHS was subject to a “Radical Reorganisation’ at the beginning of 1974. It appears, to those of us who committed our lives to it, that it has been in a ceaseless process of reorganisation ever since, with further ‘re-disorganisation’ to come. This relentless model of change: ‘The Permanently Melting Ice Cube’ model of Change-Management, can certainly challenge medical morale. A jaded starting point to begin to address the enormity of Sars-Cov-2.
But what has happened to patient-morale leading to this reported crisis in
trust, and change in public opinion?
Micro-management and Evidence Debased-Guidelines (dependent on Ghost-Written, academic-malfeasance-distorted clinical trials) with denial of ADRs such as AKATHISIA, PSSD, PGAD, and the repeated misdiagnosis of ADRs certainly erodes trust. Once damaged, trust at the level required for therapeutic patient-doctor relationships may be almost impossible to reconstruct. A spiral of descending morale on both sides of the consultation is a more likely outcome?
I had a G.P. who listened with concern and with empathy to the iatrogenic tragedy that followed inappropriate SSRI prescribing to my daughter (in a different Practice). He read publications by Professor Healy on PSSD. He learned more about AKATHISIA, and recognised this happen himself. His humility and professionalism meant that I was fortunate enough to be believed and not rejected. I realise that this contrasts with the absolute denial of serious ADRs by some prescribers, especially re psychotropic drugs. I have, I believe, also experienced such response. This leaves those with AKATHISIA; ‘In restless dreams to walk alone”. To fear that their ‘words like silent raindrops fell’. Were their doctors: ‘talking without speaking’, ‘hearing without listening’?
Then how can we possibly communicate what has happened to us credibly in ten or fifteen minutes of consultation time in a palpably over-running surgery?
‘Silence like a cancer grows’. Sounds of Silence. Now more haunting than before.
As a hospital doctor, I had more time to listen to my patients. I would like to believe that I was hearing them.
‘Will’s ‘family is hoping an inquest will give some answers. If only – when suicidal he was asking for help for his mental health problems – he was told to download a mindfulness app. Will died after documenting his distress in the hope, he said, of alerting others – alone in a squalid flat
Share this post BBC News
Posted at 0:01 27 Aug0:01 27 Aug
Video caption:
Autistic teen posted a video about lack of support in health and social care system before he died.
Antidepressant withdrawal: why has it been ignored for so long?
https://holeousia.com/in-the-world/a-sunshine-act-for-scotland/pe01651-prescribed-drug-dependence-and-withdrawal/antidepressant-withdrawal-why-has-it-been-ignored-for-so-long/
recovery&renewal
@recover2renew
Replying to @jf_moore @Reduxreloaded and 2 others
Seems quite a very deliberate ‘reframe’ / whitewash by Wendy ..
Nigel Praities: “Wendy did some research, she went to meetings, looked at the online patient forums, spoke directly with patients and GPs. And like all good scientists, in the face of mounting counter-evidence, she changed her hypothesis.”
Professor Wendy Burn: “I think the thing that really clinched it for me was GPs. So I went to a big meeting at the Royal College of GPs and we weren’t really there to talk about withdrawal, but I sort of looked round the table and said: ‘Is there a withdrawal problem with antidepressants?’ and every single GP said ‘YES’. So that was when I absolutely realised there was a problem which I had missed.”
Nigel Praities: “The College, under Wendy’s leadership, has become a major voice for change, pushing, amongst others, for a changes in NICE guidance on withdrawal symptoms, producing guidance for both prescribers and patients on how to taper
James Moore
@jf_moore
·
No mention here of all the polite and reasonable interactions that went on. No mention of the behind the scenes work to provide the knowledge that psychiatry should have had about withdrawal. The ‘scientology’ card played again. Extremely disappointing.
#antidepressants
https://missd.co/missd-presents-akathisia-info-at-london-conference/
Recollections may vary…
‘I think the thing that really clinched it for me was GPs’ — I sort of looked round the table and said: ‘is there a withdrawal problem with antidepressants? and every single GP said yes’ —
We weren’t told if a critical follow up question was asked: ‘And do you warn your patients about this withdrawal problem before you prescribe’?
GMC 5th April 2021. Update; Good Practice In Prescribing and Managing Medicines and Devices:
Assessing The Patient’s Needs.
40 You should reach agreement with the patient on the proposed treatment explaining: a) The likely benefits, risks and impact including serious and common side effects.
85 You should make patient safety your first priority.
If the prescriber has been repeatedly advised, and become convinced, that these drugs prevent suicide, it is understandable that this concept may take the first priority.
recovery&renewal
@recover2renew
·
1h
LETTER: Antidepressant Withdrawal: why has it been ignored for so long? “As patient campaigners on the topic of #antidepressant withdrawal issues, we heartily welcome this PJ podcast…some ‘patient voice’ reactions & twitter comments”
https://madintheuk.com/2021/09/letter-antidepressant-withdrawal-why-has-it-been-ignored-for-so-long/… via @MITUKTeam
https://www.madintheuk.com/2021/09/letter-antidepressant-withdrawal-why-has-it-been-ignored-for-so-long/
A letter regarding the PJ PODCAST, 26 August 2021: Antidepressant withdrawal: why has it been ignored for so long? – The PJ Pod | Podcast on Spotify.
— By Marion Brown, James Moore, Peter Gordon, Ed White, Alyne Duthie
Sarah W has since lost her seat in the UK Prliament She didn’t reply to this as neither did she to mine and no doubt others . She is married to Adrian James who became president of college of psychs . Maybe she had her eye of that prize and wasn’t going to rock that boat.
BJGP Life
LETTER TO DR SARAH WOLLASTON – PREVENTION OF SUICIDE AND CONTINUITY OF CARE
Posted by BJGP Life | 10 Mar 2017 |
David Zigmond was a small practice GP in south London 1977-2016. You can
read Obituary for St James Church Surgery here.
This is an edited extract from a letter to Sarah Wollaston MP, Chair, Parliamentary Health Select Committee.
PREVENTION OF SUICIDE. THE CRUX OF PERSONAL CONTINUITY OF CARE
Late in December I heard a radio discussion (BBC Radio 4, Today) about how our community and its designated services might best prevent suicide. All the participants, including you, talked with clear sense about evident truths: our need for adequate (and increasing) funding, the need for skilled vigilance in primary care and in charitable organisations, easy access to joined-up, well-trained specialist services… No surprises and no real contention.
What I did not hear was anyone emphasising the importance throughout pastoral healthcare – so particularly with the desperately emotionally anguished – of personal continuity of care. No substantial attention was paid to the harm done by serial reforms and modernisations which, generally, have made such personal care increasingly difficult, now often impossible.
Pastoral healthcare has become increasingly misunderstood, neglected and impoverished.
Yet recognising and understanding these losses is essential for any therapeutic reparation and engagement. Since my medical qualification more than forty years ago the medical technologies have undoubtedly got better, but the healthcare relationships that administer these are often worse. How this has happened is complex: the consequences, certainly, are unintentional. The result is that, overall, treatments of structural diseases continues to improve, but pastoral (personal) healthcare – that which cannot be quickly fixed by technology – has become increasingly misunderstood, neglected and impoverished. Within this rubric mental healthcare is a prime example.
In the 1970s I worked as a young psychiatrist. Mostly we were able to provide a kind of flexible and personally attuned care with personal continuity, which has since been driven out by modern systems. This erstwhile care was largely provided by consultant-led general psychiatric ‘firms’ together with family doctors (rather than ‘primary care service providers’) who then worked in much smaller practices with identified patients (‘personal lists’). Both provided cornerstones where patients and practitioners could, through repeated and easier contact, develop bonds of naturally evolving personal knowledge and understanding. Most sufferers of mental health problems and experienced practitioners agree that such personal continuity is essential to the kinds of relationships that can enable first, trust and comfort, and then healing, repair and growth. This work is delicate and nuanced so becomes much more difficult – if not impossible – where there is not the time or context to develop these bonds. It can be helpful to see the evolution and nature of such bonds – between sufferers and healers – as bearing a close resemblance to those that evolve in well-functioning families: both are held together by developing relationships of trust and affection.
Such a ‘family’ ethos of providing pastoral healthcare has been made more and more unviable by our successive reforms and modernisations. With few exceptions, such ‘progress’ is defined by increasing systemisation so that the vagaries of personal meaning, relationship and attachment are replaced by rapid devices for ‘logical’ process: diagnosis, despatch and packaged intervention. Influence by bespoke individual understanding becomes displaced by generic prescribed ‘treatments’. But with this kind of human complexity we usually find that the greater our efforts of direct control, the less our understanding. If we are heedless of this we risk killing – however inadvertently – the human heart and natural habitat of our pastoral healthcare.
Modernisation programmes have become – paradoxically – antitherapeutic.
This change of care ethos from a kind of family nexus to a factory-like complex of contracted ‘service providers’ has increased massively in the last two decades – the last half of my long career in Psychiatry and General Practice. In that time I have seen now both services have become depersonalised in proportion to their systemisation. What does this mean? Increasingly, people do not know one another: contacts more rarely become deeper relationships, not just between doctors and patients, but also between colleagues. Data storage and transfer may be rapid and complete, but the slower, subtler, human processes of growing meaningful attachment, affection and containment have been largely driven out by our reforms. So such modernisation programmes have become – paradoxically – antitherapeutic. Hundreds of conversations I have had with older practitioners and patients support this view – the exceptions are apologist colleagues in management posts.
What are the devices that have transformed our healthcare family into a factory: from understanding natural processes to driving industrial protocols?
One source is our illusion that we can treat healthcare as a commodity, utility or manufactured object. From this other things have necessarily evolved: a consumerist view, attempts to monetise and proceduralise all care so that it can be commissioned, traded and controlled. Hence the Internal Market, the purchaser-provider split, autarkic competing NHS Trusts, Clinical Commissioning Groups, commercial-type incentivisations, the Health and Social Care Act (2012) … the list continues to grow. We have been very clever at fashioning such reforms, but very unwise not to see an ineluctable flaw: their destructive human and social effects.
This dehumanising systemisation of services is seriously demoralising and has led to our poor staff recruitment, sickness, drop-out, burnout, premature retirement … and suicide.
Our corner-stoned 4Cs – competition, commissioning, commodification and computerisation – have all been much vaunted as assuring more accountable, equitable and efficient healthcare yet have rendered us general practice and mental health services with poorer human contact, engagement and attachment. This dehumanising systemisation of services is seriously demoralising for staff. The work becomes increasingly stressed and impoverished of deeper (human) satisfaction: this has led to our poor staff recruitment, sickness, drop-out, burnout, premature retirement … and suicide. How can complexly distressed patients possibly do well in a service that is itself so sick?
In the last few years of my work in the NHS I have found it increasingly difficult to offer the kind of personally synergistic, comforting, containing, healing work I used to manage so readily with colleagues. The reasons for this are largely found in our organisational reforms – the kind of thing I have outlined above. Potential suicides pose our trickiest and starkest healthcare questions and tasks. There is always more to think about, to do and undo.
More NICE tosh if anyone can stomache reading it….no user groups were included in the list of contributers they might if they hadn’t been brain washed or bought off with funding have pointed out that it is immoral to publish guidelines whether they can leaglly be ignored or not, (NICE leaving themselves a NICE loophole) which are not based on reliable data as DH keeps on and on and on exposing.
Shared decision making NICE guideline Published: 17 June 2021 http://www.nice.org.uk/guidance/ng197 © NICE 2021. All rights reserved. Subject to Notice of rights (https://www.nice.org.uk/terms-and-conditions#notice-of-rights).
Patrick D Hahn Retweeted
BOB FIDDAMAN
@Fiddaman
All it would take is one savvy journalist to ask Chris Witty, Patrick Vallance or Boris Johnson the right question. Why won’t Pfizer allow anyone, including the MHRA and CDC, to see the individual Case Report Forms from the on-going vaccine trials? Your Pulitzer awaits…
Savvy journalist…
GlaxoSmithKline moves another step closer to finally getting a Covid vaccine approved as drug giant starts phase three trials of one of its four jabs
No10’s chief scientific advisor Patrick Vallance was previously head of research and development at GSK.
England’s deputy chief medical officer Jonathan Van-Tam was also once a consultant for the London-based company.
https://www.dailymail.co.uk/news/article-9942567/GSK-SK-Bioscience-start-late-stage-trial-Covid-19-vaccine.html
Demand for information – known as a ‘subject access request’ – has increased since the publication of the Commission of Investigation’s report according to the company.
https://www.rte.ie/news/ireland/2021/0901/1244136-gsk-information-service/
Savvy Journalist – Escape from a ‘Paroxetine’ Maze
Ex-GSK CEO Andrew Witty to join WHO COVID-19 vaccine efforts
Ex-GSK CEO Ian Hudson Senior Advisor, Integrated Development, Global Health for the Bill and Melinda Gates Foundation.
‘Catch Me If You Can’ – the movie…
Is there any where we could rely on for good practice ? yet more publications – but little action it seems.
British Journal of General Practice
Research
Medication-related harm in New Zealand general practice: a retrospective records review
British Journal of General Practice 2021; 71 (709): e626-e633. DOI: https://doi.org/10.3399/BJGP.2020.1126
Harms from psychiatric drugs
Response from Susanne
Published on: 26 August 2021
For first hand accounts and academic publication please read Rxisk blog and David Healy blog of McMaster University.
http://antidepaware.co.uk/millie-and-the-tsar/
Dear Mrs Doherty
Thanks for replying. I want to try to answer your questions in the most helpful way, so it makes sense to start with my understanding of the main issue you have raised.
SSRI antidepressants can cause akathisia. I have seen many patients with akathisia, caused by different drugs, and it is an extremely unpleasant condition that at its most severe can make people feel desperate and suicidal.
It’s hard to estimate how often it causes suicide or self-harm, partly because what makes people suicidal is often a mixture of problems – it is rarely caused by one thing. However, the risk is sufficiently concerning for us to be cautious at all times, especially when starting or stopping treatment. It’s essential that the doctor who prescribes SSRIs should inform the patient about this risk, as you say, though I do understand that doctors don’t want to put a patient off taking treatment & getting the balanced message of risks and benefits right can be hard.
On the national suicide prevention strategy, I need to explain a little of the background. When we came to update the strategy a few years ago, the Government wanted as few changes as possible. We were keen to add something about antidepressants after hearing from families who felt strongly about this and we thought it was best done in the section on treatment of depression in primary care which was mainly about the risks of getting no treatment. So we added a line to the key messages of this section, as follows:
“There are also risks in the early stages of drug treatment when some patients feel more agitated.” (page 27).
This may not sound a lot but at the time it seemed an important and unusual acknowledgement to appear in a Government strategy. We used “agitated” because it was a document for the general public rather than clinical guidance for doctors – that’s the job of NICE – or information for patients, which is overseen by the regulator, the MHRA. Current NICE guidance says something more specific about the need for careful monitoring in the early period of treatment, especially in younger people, because of suicide risk.
I’m sorry to hear about the difficulties your step-daughter has faced. If she has had severe akathisia on withdrawal, it’s an important point of safety to withdraw more slowly, to avoid the distress I’ve mentioned. Most people can come off antidepressants if it’s done over the right time period, and that can vary for different people.
I hope I’ve answered what you were asking about your step-daughter but if I’ve misunderstood please feel able to come back to me. Of course, I’ve “unblocked” you – happy to do this – but being in touch by email is a lot better than twitter.
With best wishes
Louis Appleby
https://fiddaman.blogspot.com/2019/10/uk-suicide-expert-akathisia-can-make.html#.YTHzEfeSk2x
Record numbers of children are being prescribed antidepressants
Kat Lay, Health Editor
Tuesday August 31 2021, 12.01am, The Times
Children are being prescribed antidepressants in record numbers, new figures from the NHS reveal. In 2020, there were 231,791 prescriptions for the drugs issued to children aged between five and sixteen.
https://www.thetimes.co.uk/article/record-numbers-of-children-are-being-prescribed-antidepressants-88268m0rt?mc_cid=d2b3caea3d&mc_eid=UNIQID
Rxisk is still there…
As someone who was put on antidepressants at age 13, now 23 years ago it really hurts me to see that this is a practice that is still continuing and to see it is not just limited to my own country (Belgium).
It remains impossible to understand that while the information is available on this site, in an accessible way it still doesn’t get through to the people making those decisions.
It’s not that the information isn’t in other places either. I was recently looking through the guidelines of the Belgian pharmacologists who basically publish the book/site that every doctor has and it’s actually in there. On occasion I have seen them link to for instance Rxisk with regards to the recognition of the EMA on PSSD. It is mentioned if I interpreted it correctly that psychotherapy should be the default treatment for depression.
Recently here there had been an announcement that psychotherapy would be covered more by the government health insurance system and that a session would end up being more affordable (you’d get 20 sessions at the price of € 11/per session instead of the default € 55). Turns out it’s only in a trial phase currently so extremely limited. Just an empty promise again.
For governments who only look at the short time it remains much easier and cheaper to “subsidize” medication and the consultation of the pill pushers instead of investing in the better long term outcome of the patients. Not seeing that getting people better has a much higher impact on their budget. Less costs for disability/unemployment and so much more.
And importantly they seem to forget or is it ignore, that the most important thing in medicine should be to do no harm.
I’ve been lucky that after so many years I’m now in a situation where I can afford a private psychologist and the progress I’ve been making in the last year is huge. Compared to the 20+ years on psychopharma cocktails.. Thanks to all of those who are still fighting against this, listen to their patients and give them a voice!
Generation Sedated: why record numbers of our children are on antidepressants
The number of young people taking pills is rising, even though GPs aren’t supposed to prescribe them. What does the science say?
ByMiranda Levy4 September 2021 • 5:00am
https://www.telegraph.co.uk/health-fitness/mind/generation-sedated-record-numbers-children-antidepressants/
The number of children on antidepressants has soared. Is it a real crisis or one invented by psychiatrists seeking new patients?
https://www.rt.com/op-ed/534062-children-antidepressants-psychiatrists-crisis/
The medicalisation of childhood is one of the most depressing features of Anglo-American child rearing. Year by year, it’s getting worse.
The problem of mental health is fast becoming synonymous with childhood. Unfortunately, the medical establishment is more than happy to solve the problems of children by shoving drugs down their throats. This alarming trend was highlighted by new NHS figures published at the end of last month that showed that prescriptions for antidepressants given to British children aged 5 to 16 has risen by 22% during the past five years.
Predictably, the prescribing of antidepressant drugs has spiked since the lockdown. The tendency to medicalise children’s behaviour has intensified since the outbreak of the coronavirus and sedating them is frequently regarded as the most effective way of dealing with their problems.
Frank Furedi’s 100 Years Of Identity Crisis: The Culture War Against Socialisation is published by Routledge Press later this month.
Question More…