Never before in human history have so many had to entrust
their lives and wellbeing to so few and been so betrayed.
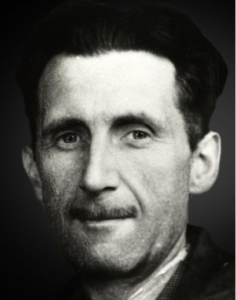
Inspired by Winston Churchill
The further a society drifts from the truth
the more it will hate those who speak it
Inspired by Winston Smith
Probity Blockers, a term originally coined by Dee Mangin, were a big talking point on RxISK in 2024 and previous years – along with Trans Medicine. Both have featured in posts on DH and RxISK since posts began in 2012 – See 101 Uses for a Dead Journal and Getting my Doctor to Disclose.
The problems with probity blockers came to something of a head with the death and recent inquest of Thomas Kingston as they do with all drug induced deaths and inquests – Shane Clancy, Dexter Johnson, Sam Morgan, Romain Schmitt, Darren Connell and others.
Professionals
Around the time of the French Revolution medicine joined law as a profession. The definition of a professional, whether a lawyer or later a physician, was to be a point of access to advice that was independent of Church or State.
Law had led the way in this respect. It was central to the development of nation states, especially following the creation of the printing press, when the amount of available information increased exponentially, and it made sense to have someone able to help us get to grips with what might work for us from among a growing range of options.
Medical professionalism was caught best by Philippe Pinel in 1800 when he said that it was great to have treatment options but an even greater art to know when not to use them. A good relationship between a person with a problem and a professional they consult is central to knowing when not to start or when to stop something.
The later development of treatment techniques, especially in the wake of the American Civil War, to which medical professionals might turn created a tension that was initially most clearly apparent with surgery. New equipment and developing anesthetic capabilities tempted surgeons down the route of doing more and ever better operations from which patients died.
Rather than serving us, like boy racers or mountaineers, there was a sense that faced with a cancer or other disorder surgeons were more taken by the thrill of engaging with an old adversary and were liable to lose sight of us.
Technologies are rarely, if ever, tools that we can employ without being affected by them. They invariably lead to developments we never imagined when first put to use for the purpose that led to their invention. Plastic surgery aimed at rehabilitating soldiers injured in World Wars became cosmetic surgery after the Wars.
In this medical technologies resemble A.I., which even before we start using it confronts us with profound questions about our abilities to make it work for us rather than have us work for it or those who stand to gain by it.
Bullets or Magic
As caught in the phrase surgical strikes, surgical technologies are relatively clean compared to the drugs that came later. While creating a Magic Bullet was the guiding imagery behind drug development, the reality was nothing like this. Many of the new medicines affected every system in the body and for most of them we still have little idea about their full range of actions.
A hundred years ago, physicians set themselves up as a bulwark against the panaceas being pushed by fly-by-night pharma companies. Medicine promoted the idea that the Magic lay in a good Doctor rather than in any of these ‘nostrums’ which either contained nothing or else a range of harmful substances.
In 1914, physicians seemed like just the right kind of responsible professionals to be entrusted with a police function, when the Harrison’s Narcotics Act made opioids and cocaine prescription-only.
The antibiotics of the 1930s inaugurated a new era of potentially effective medicines. They also set up a clash.
From the first Food and Drugs Act in 1875, companies were required by law to state the contents of a medicine in its label and make some claims about its use. Previously physicians sent details of the medicine they wanted the patient to have on a prescription to a pharmacist to be compounded – our treatments were bespoke to us.
Companies inserted themselves into this doctor-patient relationship when they argued for making all new ‘ethical’ medicines prescription-only. Otherwise, companies argued, they would have to put an entire medical course on the label of these new medical drugs and no lay person was going to understand instructions like “give this drug for this but not for that” or “do not combine X with Y”.
Few if any doctors were to know that the relationship between us and them was about to change. S/he was no longer giving us something bespoke to us. The information s/he brought to bear on the help s/he might give us had been based on her experience of what worked and her knowledge of us, but s/he would soon be giving an off-the-peg product and would be told that her experience counted for nothing.
This initiated a process that led to Pharma dictating what experiences on their drug are valid and what aren’t.
A Tragedy
Around the time the thalidomide crisis broke, doctors were openly contemptuous of the bureaucrats who regulated medicines. When framing the Amendments to the 1962 Food and Drugs Act that introduced Randomized Controlled Trials (RCTs), legislators – politicians were at pains to stress they were regulating claims pharmaceutical companies make about their products – they were not regulating the practice of medicine.
It took the bureaucrats two decades to sort out how to make RCTs work as a regulatory tool. By 1980, regulators figured they knew more about RCTs than any doctors. As soon as RCTs became the eye of a needle through which drug camels had to be squeezed, companies had an incentive to make sure they knew more about RCTs than either bureaucrats or doctors.
Beyond the fact that the medicines we got from our doctors had brand names, and were available on prescription-only, there was little difference in the practice of medicine between 1950 and 1980 when RCTs came into play.
If the bureaucrats and companies were and are correct in their views about the limited abilities of doctors to understand key things that affect them like RCTs and prescription-only, and they appear to be, what has been happening since speaks to an extraordinary mendacity on one side of a growing crisis and on the other medical side an unbelievable naivety, and a misbranding of physicians as professionals.
The word tragedy refers to a catastrophe that is self-inflicted. Louis Lasagna had been the main American advocate for RCTs in the 1950s and 1960s and was responsible for their introduction into the 1962 FDA amendments as a means for companies to test their medicines for effectiveness. The fact that a physician was responsible for our unfolding catastrophe makes this a tragedy – The Tragedy of Lou Lasagna.
In the 1980s, when RCTs were finally adopted we saw the first claims that RCTs were the sophisticated way to establish reliable information on the side effects of drugs.
Claims like this drew a wonderful response from Lasagna.
This may be true in the dictionary sense of sophisticated meaning ‘adulterated’ … spontaneous reporting is more ‘worldly-wise, knowing, subtle and intellectually appealing’ than grandiose, expensive RCTs.
This emerging company narrative was weaponized 8 years later in response to a knowing, subtle and intellectually appealing report on fluoxetine triggered suicidality from Martin Teicher and colleagues.
Availing of BMJ complicity or Richard Smith’s, BMJ’s editor, naivety, Lilly responded that the views of Teicher and his colleagues, along with the views of 20 or so other academic groups, were anecdotal. RCTs were the science of adverse event cause and effect. – See Truth, Trust and Health.
This flew in the face of everything Austin Bradford Hill, the creator of RCTs, said about them. It was completely at odds with everything Lasagna said once he realized the error of his way in advocating for RCTs in the way he once had. Astonishingly, however, with extraordinary rapidity this worm wormed its way into the heart of medicine and undermined doctors’ confidence in their ability to practice Evident Based Medicine.
The worm branded as Evidence Based Medicine looked plausible but this was the birth of Trans-Medicine.
Medicine that Ignores Us
Knowing everything about the pharmacology of a drug – what side effect occurs at what rate in (company) assays – see Health’s Illusions – is not the role of a doctor. Even an expert who focuses on just one drug is likely to hear new things that drug does in most clinics s/he runs. The role of a doctor in a clinic is to keep a person who brings a problem to us as safe as possible in the midst of uncertainties.
When we take a problem to a doctor, we are like someone who has to get somewhere fast in dangerous weather on an icy and dark road known to be lethal. Given a choice between being driven by an automobilologist, who knows everything there is know about cars, or by someone who is the best driver you know, who has driven this road before – which do you pick?
You want someone who is alert to everything happening on the road, things you may not spot, someone who figures your input can be critical, if for whatever reason you need to take over the driving, help retrieve the care from mud, or change a wheel.
Your clinical input is more important than a passive passenger role, but my point here is about the driver. The situation on this icy night is specific and the key skill lies in dealing with uncertainties. It’s about real life competence not book knowledge. In a clinic it’s being able to work with the privileged observations of the person being poisoned which although done for the best of reasons is always dangerous.
It would have been shocking and rare in the 1980s to hear any of us say our doctor was gaslighting us. Now it is extraordinarily common.
We now have more and more policy documents insisting on the importance of the patient’s voice and that of their families – provided neither speak about the adverse effects of medicines. See Is Your Treatment Making You Suicidal.
Professional in Name Only
For close on two decades when speaking to medical audiences, I’ve made the point that if our meds work as well as the hype claims and are as free of hazards as EBM states, then doctors are out of business. We will be replaced by cheaper physician associates (PAs) and nurse consultants.
This is now happening at pace. Medical journals and lay media are stuffed with accounts of medical complaints about PAs and others leading to an increasing toxicity in healthcare settings. The BMJ is full of the issue this week – One, Two, Three.
This is delicious if only because for over a decade BMJ (and other medical journals) have gone out of their way to Silence Doctors. Articles on drugs and their hazards now get written by journalists, as the lawyers for medical journal’s fear that even the shadow of a doctor falling on an article about a drug might lead readers to think the journal was really supporting claims this drug causes that problem.
Fiona Godlee, the BMJ editor who followed Richard Smith, professed an interest in publishing the Restoration of Study 329, the study that more than any other demonstrated how companies go about hiding adverse events, but had to be dragged to the publication. Liz Loder, the BMJ editor put in charge of shepherding it out of existence it seemed – was married to a lawyer working for Ropes and Gray, a Boston law firm who defend GSK.
Well before the BMJ showed how scared they are about adverse events, 101 Uses for a Dead Journal was a 2012 DH post. 101 Uses for a Dead Profession would have been an equally appropriate title. This post aimed at an amusing tone, although the sheer petrification of our professional journals is laughable but not amusing.
Even earlier again, in 2004, the American Psychiatric Association posted what I routinely describe as a suicide note. Alarmed at an FDA hearing that had to concede that the trials done of antidepressants in minors, in addition to failing to show a signal for efficacy, returned a doubling of the suicide event rate on active treatment, the APA rushed out a statement claiming APA believe that Antidepressants Save Lives. They didn’t have the wit to say Psychiatrists Save Lives.
Ditto the Royal College of Psychiatrists Suicide Note
The contagion spreads beyond professional bodies like APA, RCP and their journals.
From the late 1990s onwards, I have participated in inquests for people triggered to take their own lives by the antidepressant they were on – Shane Clancy, Stephen O’Neill, Sam Morgan, Dexter Johnson, Darren Connell, Tom Kingston and many others. At these inquests, in order to avoid a later legal action against him/her, the doctor who prescribed the drug is ordinarily advised by his medical defense insurer to deny the drug has caused the problem. Or his lawyer may arrange for him not to attend or will do the talking for him.
The medical side to an inquest will find this 4 minute video, which gives some sense as to how the system works, comforting. Families who have been there will find it shocking.
You can download the video from here:
https://drive.google.com/file/d/1UvQfrqQUfQALSYQY44GSzdekqbOZLE-t/view
At an inquest, a medical professional should feel a fiduciary duty to the dead person and their family to spell out what s/he thinks the cause of death likely was. At or before an inquest is a time for a doctor to do the right thing by those who have suffered a grievous loss, rather than to focus on, or let lawyers focus on, saving the doctor’s skin.
There is more than just honesty to a grieving family involved. If the coroner figures it’s as plain as day the medication caused the problem and sends a Preventing Future Deaths or the equivalent report to regulator (the MHRA in the UK), the regulator is likely to respond and ask – well what did the treating doctor say? If the treating doctor has said nothing about the cause of death, the regulator will say they can do nothing about the situation.
Katinka Newman in a recent article on Tom Kingston’s death figured she should ask MHRA about this and got Dr Alison Cave, Chief Safety Officer at the MHRA who told Good Health: ‘As with all medicines, SSRIs have the potential to cause side-effects which are described in the product information leaflets supplied with the medicine…
‘We always remind patients not to stop taking any medication without talking to their healthcare professional first.’
This is a recipe for suicide on a mass scale. Young and old, women and men, will continue to die and regulators will continue to wash their hands – unless doctors like those treating Sam, Tom, Dexter and others stand up and make it clear the only reasonable way to explain this death is the drug caused it.
The product information for the drugs does not come clean on any of the serious risks linked to these drugs – not just the risk of suicide. There is no mention of drug induced alcoholism, homicide or even permanent sexual dysfunction. Regulators make it clear they do not want to deter people from getting the benefit these drugs can offer. If they ever change their mind on this it will be because pharma figures they need to get rid of these old cheap drugs and some decent warnings might help them with this.
Doctors aiming at keeping us safe should pay little or no heed to drug labels written by companies and endorsed by bureaucrats. Doctors who see the problems should be telling regulators what they require to be in the labels – especially now that brave medical journals like BMJ absolutely refuse to have articles by doctors about the hazards of drugs.
If there were any medical leaders they would never have let us end up believing that public safety depends on a bunch of bureaucrats.
I was interviewed on Times Radio following the Kingston inquest and the interviewer pushed me to agree antidepressants are very safe with rare side effects. Agreeing to this will put me and all doctors out of business, but most doctors roll over and agree.
Physician Heal Thyself?
The only reason medicine survives as a notional profession is because it suits pharma. Doctors are a convenient fall-guy on which companies can palm off legal liability.
Are doctors professionals?
The hallmark of a professional is the advice they give. Doctors no longer listen and offer bespoke advice – they read from a script. Unless your antennae have been numbed, it is easy to sense all the others in the room with your doctor and you when you bring him a problem – Strangers in the Room – Managers, Guideline Makers, Ethicists, Journal Editors, and as of last week Baroness Gillian Merron, the British Under-Secretary for State for Mental Health, who in the House of Lords said:
However, a prescription is made only after discussion with the patient about it and other alternatives, and the clinician has to follow and comply with the guidelines.
Gillian almost certainly hasn’t read The NICE before Christmas and is likely speaking in all innocence here. When does innocence stop being a defense?
Are doctors bureaucrats?
Bureaucrats, such as medicines’ regulators, adhere to protocols. They never lead. Anyone looking to FDA or MHRA or EMA to lead is looking in the wrong place. It is not part of their job description or their DNA.
Leadership comes from leaders. Politicians can lead – can insist on something being done and the bureaucrats have to hop to do so. The politicians get constrained by pharma threats to pull out of their country with the consequent job loss etc, if they insist on Cisparency. Transparency is no problem – we know that the public finding out that key opinion leaders are paid by us causes no problem. See Cisparency or Transparency.
With vaccines the new cash cow, and the removal of Democrat patsies in the U.S., the UK must look very appealing to pharma. “Wes” (Streeting – new UK Labour Minister for Health) – “we can vaccinate everyone at birth for everything – cancers, drug abuse etc not just infections – and the NHS will cost only a fraction of what it costs now. Let us help you Embrace Healthcare’s Opportunities.
The leaders for medicines safety – and effectiveness – were supposed to be doctors not bureaucrats or politicians. But doctors are not leading. They are following what is prescribed to them from above – and as Gillian tells them they now have to do prescription-only things.
Are doctors technicians?
In contrast to professionals, technicians have gadget skills. Surgeons are the gadget guys in medicine – or were until robots began to take over.
An old adage was that surgeons’ would say about doctors ‘Don’t stand there, Do something’, while physicians would say Don’t just Do something, stand there. But even though into gadgets, these days many surgeons are more likely to take time to gauge their patient and whether going ahead with an operation is the right thing for this patient
Technicians, even athletes, become professionals by virtue of being paid in contrast to amateurs. Doctors certainly get paid more than other healthcare professionals.
Are Doctors Salesmen?
the job description doesn’t say so. But pharma have close to completely got rid of their sales force and depend on doctors to sell the product. Doctors are the best-paid salesmen around but we who pay taxes or insurance premiums, or both, pay their wages – so pharma get a sales force for free.
Although not paid for by companies, as company doctors are, doctors still have a feature that effectively makes them company doctors. Company doctors are liable to lose their job if they mention that the company drug has hazards. So to with doctors in health service companies – even publicly paid ones like Britain’s NHS.
Trans-Medicine
As opposed to regulators of medicines, there are bodies that regulate medicine. In the United States is a set of boards that certify doctors. In Britain, it is the General Medical Council (GMC). Doctors who get investigated by the GMC and the various other boards are said to turn grey-haired, have serious illnesses, get divorced and commit suicide.
GMC in particular accept they have a track record of being manipulated by trumped up charges from the managers of health systems and others in positions of power to take actions against doctors who raise safety concerns about medicines or other clinical practices. Other medical regulators in the U.S., Canada, Australia, Europe and elsewhere can be similarly manipulated.
In addition to ensuring doctors do not speak up about adverse events, GMC otherwise come down heavy on doctors who might be over-friendly with patients – usually not on the scale of the friendliness of Xtian or other religious clergy.
In Britain, ably assisted by BMJ and BMA, GMC played a prominent part a decade ago in warning doctors that they risked being struck-off if they didn’t give puberty blockers to minors who wanted them.
A journalist approached a colleague recently who reported him as saying:
I spoke to one doctor yesterday who said he felt bewildered by the complete capture of our evidence-based institutions and the culture of fear about speaking out which he thinks is causing harm. I’m looking for specific examples!
This journalist was trying to find out what doctors think about puberty blockers and the current state of transgender treatment.
Whatever anyone else’s views about transgender states, the transgender story illustrates how easy it is to capture the highest echelons of medicine – to capture the great and the good. Cis-Medicine was captured in a matter of months in the early 1990s. Despite falling Life Expectancies and Reproductive Rates, there are almost no signs that anyone recognizes what happened.
Well-meaning but naïve medics intone their concerns about regulatory capture by which they mean capture of FDA, EMA etc – capture of the regulators of medicines. This is not our problem. The problem is the capture of medicine which in 1962 was envisaged as continuing to be the primary regulator of the safety of medicines in practice.
Several colleagues have lodged complaints with GMC about doctors who have had medical research papers ghostwritten for them – essentially fraudulent representations of the results of studies on life-threatening conditions made worse by treatments from which pharmaceutical companies have made billions. GMC have responded that this is outside their remit and have done nothing.
The Right Stuff?
The extraordinary feature of this story is that no group of people have ever been handed such power to keep others safe as doctors have been handed.
Making modern medicines prescription-only gave doctors the power to refuse to prescribe them without access to the data, or if the price is too high, or if companies or regulators refuse to amend the labels to include the problems doctors see in daily practice.
Power like this means that medical journals like BMJ or the New England Journal of Misinformation could print whatever they want without a care in the world. Threats from pharma’s lawyers could be managed by saying we will run an article about these threats and we’ll see how many of our medical readers continue to prescribe your drugs. Pharma’s threats are bluffs. Bluffs are all they need. They know Medical Journals are so Eli Lilly-Livered that they will cave in before the email even gets to them.
There is zero sign of medicine getting its act together to bring about meaningful change. Zero sign that doctors are made of The Right Stuff.
Doctors preen themselves on the purity of their good intentions, and their nobility forged from witnessing so much suffering. The suffering of others. Everyone else is wrong except them.
There is an old saying about salt – what use is it if it loses its saltiness. We don’t need our doctors to be saviours but we do need them to be savoury/ salty. See Can Doctors Save their Jobs and the World.
Life expectancies and reproductive rates are now falling across the developed world – an inevitable consequence of clinical practice being based on a fraudulent literature aimed at supporting the health of companies rather than folk who come to a doctor in need of professional input.
In the near future, we will wake up to this crisis. See The Right Stuff – The RxISK Stuff.
Do we have to let the luxury liner, HMS Medical Profession, sink beneath the waves to the sound of recriminations, whimpering and whingeing, with little, if any, of the Right Stuff on view to solve the crisis?
Is there any of the spirit left in medicine that made it a revolutionary force in 1789 and 1848?





We’ve touched on this before, but one way of understanding this medical dystopia (real, mind you, not imagined) is by looking through the lens of ALIENATION.
Commonsense adaption – not academic/intellectual. But Marx’s concept of alienation, the rot of capitalism, defined as the separation of workers from the products of their labour – certainly rings true for doctors. And Marcuse’s advanced industrialised alienation – ‘anaesthetization— a deadening of the senses that makes repression and manipulation possible ‘ – resonates across the system.
https://www.bu.edu/wcp/Papers/Educ/EducReit.htm
No wonder many, not all , good and caring doctors have become disconnected from their clinical senses – and their patients. It is a tragedy.
Surgeons are different – as you suggest. Even though partialists, for some reason they often seem to pay more attention to the whole person. Particularly with serious interventions – thinking Henry Marsh and brain surgery – there tend to be a string of consults where relationship medicine forms. And I guess cutting into another person’s body is an intimate act.
Conversely, nowhere is the alienation more potentially destructive than in psychotropic medicine where, as you say, understanding some theoretical mode of action isn’t the answer, rather listening to and closely monitoring the experiences of the individual patient.
If doctors and psychiatrists knew how to listen – over 60% of patients in withdrawal wouldn’t have been diagnosed as relapsing or developing some other ‘mental health ‘ issue in the recent Cosci study.: https://www.madinamerica.com/2024/09/antidepressant-withdrawal-commonly-misdiagnosed-as-mental-illness/
Arguably, the presceibedharm community wouldn’t exist.
Having said that – who are the crusaders with the greatest chance of altering the course of this mess? Harmed patients. Because, as you know, having cared for them for decades, they are the people who understand precisely the adverse effects of medication on their minds and bodies. No aliention from self there at all – but often a lot of suffering
This could start the ball rolling and help Doctors and Patients, Wake Up and Smell the Coffee.
Well Done, Harriet.
RxISK not slow in pushing ahead with such an idea.
If I was a ‘slow learner’ doctor, I would think ‘blimey’, this is a very clever patient, and certainly something I never knew about. It could change the entire dynamics, of the ‘relationship’ which has been particularly ‘unhealthy’ of late.
https://rxisk.org/pro-forma/
‘We know it can be daunting facing a doctor when it comes to medication-related issues’.
Did you know SNOMED, is demons backwards…
Getting this in your Medical Records could be a life-changer.
I remember taking in a communication I received from Richard Brook of MIND; the doctor put it in my MR’s, with no fuss. Richard was very kind to write to me.
http://news.bbc.co.uk/1/hi/programmes/panorama/3710380.stm
Extraordinarily impactful, 22 years; searching questions, searching answers. Some early groundings, making waves.
Me, Myself, and Super-Me: An Interview with David Healy
The rise of the lifestyle drug
David Serlin and David Healy
Fall 2002
https://www.cabinetmagazine.org/issues/8/serlin_healy.php
David Healy: An awful lot of the frustration with health care now has to do with just this: patients have become, in a very real sense, hostages in ways that they weren’t before. People weren’t treated like addicts in the past. And physicians have become prescribers in a way that they weren’t before. They’ve often failed to recognize the dynamics of what happens when people come for treatment. And while scientists have become very good at assembling evidence on the efficacy of pills, physicians haven’t made the same developments in being able to listen to patients and make sure that they’re on the same wavelength. Now it’s done much more according to algorithms and protocols; there’s very little sensitivity in the interchanges between the physician and the person coming to see them. People have a legitimate fear now that physicians are only offering them certain drugs because a representative visited the doctor’s office from one of the pharmaceutical companies shortly beforehand. They feel vulnerable that they’re getting this pill only because the doctor is on his way to some “conference” in the Caribbean.
Annie
You dig up some of the most amazing material. This is from a long time back. I’m sure everyone will be encouraged by how much progress we’ve made
David
I caught this interview with David and Rodney on 17th. It was from New Zealand.
I thought Rodney was such a lovely man. He was so respectful, so polite, so aghast at deaths in New Zealand of youngsters. Rodney powered on with so many questions. All in all it was a delightful conversation, of our times. What I took most from this conversation was David’s urge for Rodney to discuss matters with Dee Mangin, herself a New Zealander.
From all I have seen from Dee Mangin, she is one of the most attractive, one the most positive voices of attractive reason, that one could possibly hear. Let’s hope Rodney, if he is worth ‘his salt’ talks a little with Dee, to gain even more understanding, of the upending trend, in ‘hiding the bodies’.
Also, good to see, Rodney, update his site, with most up-to-date posts.
https://realitycheck.radio/replay/dr-david-healy-british-psychiatrist-author-the-influence-of-pharmaceutical-companies-on-medical-research-and-potential-deadly-side-effects-of-antidepressants/
Evidence-based Coronership
“A shared decision was undertaken to put [him] on mirtazapine at 15mg and to follow up in 4 weeks time. I was informed that this was considered because of its side effects of sedation and increased appetite. A full mental state examination was undertaken which did not identify any Self harm or suicidal concerns.”
“There was no concern from the GP when he called 2 days later to ask to increase his medication”
“Further there is evidence that even if medication had been increased it could have taken up to 4 – 6
weeks to show any benefit.”
https://www.judiciary.uk/prevention-of-future-death-reports/david-stables-prevention-of-future-deaths-report/
Coroners tend to believe what they read in GP reports ghost-written by their Protection Gangs.
Someone else commenting on all of this earlier today said that the entire Evidence Based Medicine apparatus is there for legal defense purposes. It began in Pharma’s defense. Extended now to family doctors, it leaves them – as the legal fiction calls it a learned intermediary (risk manager)- more exposed than Pharma but somewhere you’d figure there is a realization that we don’t want to start prosecuting doctors or they might wake up and start protesting
D
The study (note my use of the singular) that served as the basis for foisting puberty blockers and cross-sex hormones on tens of thousands of children throughout the developed world looked at seventy children who were put on these drugs. All went on to cross-sex hormones, and fifty-five of those went on to have sex reassignment surgery. All were provided with psychological support as well as drugs. Then, the researchers ticked a few boxes on some symptom checklists and found a ‘statistically significant” improvement in a few areas.
Compared to what? Compared to nothing. There was no control group provided psychotherapy alone. My freshman students could explain why this study proved nothing about the efficacy of “gender medicine.”
Even these puny results have not been replicated. The researchers at Tavistock tried to replicate this study and found “no changes in psychological function” (their words, not mine) in the subjects. They sat on the data for five years before publishing them. And just last October, the paper of record reported that a UCLA study of puberty blockers “did not lead to mental health improvements, most likely because the children were doing well when the study began” (again, their words, not mine). Nine years after it began, the study remains unpublished for fear that the data (which we paid for, I might add) will be “weaponized” (once again, their words, not mine) by opponents of gender transition.
And now I see people turning on their fellow citizens who question this with the same offhanded viciousness of the crowds in Shirley Jackson’s “The Lottery” — just as they did with the mRNA shots which did not prevent infection nor transmission and which INCREASED the rate of serious adverse events.
Patrick
An important point but you make me worry I have confused people by introducing Dee’s term Probity Blockers. This post is not about transgender medicine.
That said there is a lot about transgender medicine that copies what Pharma does – which is the ramp up the terrible consequences – the perceived risk – concerns about a notional hazard – of a condition like restless legs syndrome or acne or whatever for which they want to sell their product and then totally obliterate the perception of hazards when they occur – it’s not just the perception of hazards that might rarely occur – it’s the perception of hazards happening right in front of a doctor who can no longer see them as hazards linked to the medicine is has dished out.
David
These powerful words capture exactly the deep sense of BETRAYAL caused by psychiatric serial misdiagnosis of ADRs and the ritual, cavalier, enforced prescribing of unnecessary toxic, mind and body crippling psychotropic drugs that left our loved one ‘Drug Wrecked’.
BETRAYAL reinforced by the ritual failure of those claiming to be members of my own profession.
Our society has indeed drifted, far from the truth as a result of psychiatry’s propaganda: –
marketed as science, whilst in reality: -science fiction.
It leaves society in danger of loosing trust in all doctors, and hence, at great risk when illness and disease of known and reversible aetiology affects us and our families.
‘Her financier husband, 45, who she married in 2019, shot himself dead at his parents’ Cotswolds home after an adverse reaction to anti-depressant medication.’
https://www.dailymail.co.uk/femail/article-14216329/Kate-Middletons-touching-gesture-grieving-Lady-Gabriella-Windsor-Christmas-Eve-carol-concert.html
The problem I have with articles like this, spread over most the media, is, it almost normalises the ‘shot himself dead’ after an ‘adverse reaction to antidepressant medication.”
Before going on to describe ‘Festive events’ of the Royal Family.
Which is the story?
While many are trying to focus on the dangers of psychotropic drugs, is it too much to ask that journalists either write one story or write the other. The Daily Mail are very fond of Katinka Newman and her dynamic journalism, but sometimes, are less fond, when a different story comes along?
Wouldn’t it be nice, if the the press had consistency, if Thomas Kingston, deserved more than a cursory sentence, in the battle for stories. If Tom, heralded a new era, in the disseminations of the press, choosing which stories take precedence, in their quests for reader’s attention.