Editorial Note: This is the fifth is the Lasagna series of posts that began with Not So Bad Pharma, April Fool in Harlow, The Tragedy of Lou Lasagna, Empire of Humbug: Bad Pharma and will continue through to Brand Fascism and Witty A: Report to the President.
In 1954 soon after his article with Beecher put the placebo on the map, Lasagna was recruited from Harvard to Hopkins. Beecher pleaded with him to stay in Boston.
“Now that I am faced with the unhappy fact that you are gone, I find it more depressing than I can say…. If your future career is anything like your performance here it is bound to be spectacular.”
Lasagna ended his days back in Boston, leading a Center for the Study of Drug Development, whose brief was to foster the development of specific treatments for specific conditions. In 1980, he was made president of the American College of Neuropsychopharmacology. The placebo had vanished from his working life.
Michael Shepherd had at one point been expected to take over the lead of Britain’s Maudsley Hospital when Aubrey Lewis retired but his style was too much at odds with the developing medico-pharmaceutical complex for this to be possible. He had been Vice-President of the World Psychopharmacology College (CINP) but by the mid-1960s he was persona non-grata within psychopharmacology.
He turned to primary care research and accidentally created a market for the SSRIs in the process. He grew increasingly opposed to the notion of specificity in medicine, and turned to exploring the placebo.
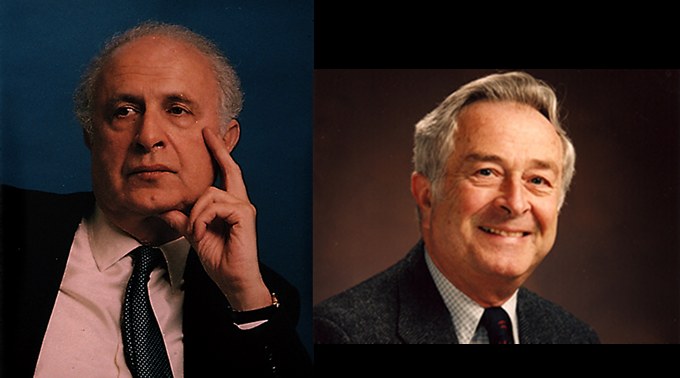
The two men met for the last time in 1992 at the 50th American Psychosomatic Society meeting in New York. Lasagna was chairing, Shepherd speaking. His topic – The Placebo (see Empire 1). [Shepherd is on the left]
When the lecture finished, Lasagna said: “this paper is now open for questions”. Nothing happened. Half a minute elapsed, a minute elapsed and nobody said anything at all. In Holland this would be normal – in America it was plain bizarre. Lasagna then said that in the circumstances they would have to move on to the next paper but he couldn’t refrain from commenting on this unnatural silence.
“There are 3 possible explanations” he said. “First you were all asleep and therefore you heard nothing. Secondly it was so bad that since this speaker has come 3,000 miles you didn’t want to embarrass him. Third it is genuinely so original and new that you don’t quite know what to make of it. I’ll leave you to decide which it was”.
What had Shepherd said?
Mirage in 1962
The key point is that little was known about RCTs or effectiveness in 1962. RCTs appeared in a late night political haggling session as a simple solution to an extraordinarily complex problem. But to paraphrase HL Mencken, like Lasagna also based in Baltimore, every complex problem has many simple solutions – all of them wrong.
Coming as he did from a position of running studies on internal states such as pain or on sleep induction, the inclusion of controlled trials late night in ’62 may not have hit Lasagna as problematic – even though in his hands imipramine, a far more potent antidepressant than any SSRIs, could not be shown to work in a controlled trial.
Analgesic and hypnotic effects were determined by means of rating scales. These effects were demonstrations of efficacy rather effectiveness against a pathological state. A demonstration of analgesic efficacy is consistent with FDA regulations that a drug be demonstrated to have an effect on a structure or function of the human body and analgesics are licensed on this basis to this day, as are hypnotics, oral contraceptives and a range of other treatments.
It would have been entirely possible to bring antipsychotics, benzodiazepines and SSRIs on the market by demonstrating their tranquilizing or anxiolytic properties. This focus would have put a premium on later teasing out what is distinct about the anxiolysis in each case – something that clinicians today quite astonishingly still cannot do although the experience you or I have of these drugs is entirely distinctive – we can easily tell them apart.
In contrast the SSRIs have performed so miserably in effectiveness trials that there is intense debate about whether they work. Half of the trials undertaken show a rating scale only differentiation from placebo. The other half shows nothing.
If in contrast, SSRIs had been licensed on the basis of an anxiolytic effect, the question of how and when to use these drugs as a therapeutic principle for depressive or anxious states would have been a separate matter that could have been tackled by the medical profession after these drugs came on the market.
Instead the effectiveness criterion has made medical conditions into a target for treatment and in so doing it set these conditions up for capture by pharmaceutical companies and their marketing departments. The effectiveness criterion created the inevitability of what is now called disease mongering.
To have to fish for possible effectiveness in some heterogeneous clinical condition is not what controlled trials were designed for. Controlled trials discover nothing. Even worse, the effectiveness claims for many drugs rest on minor surrogate marker or rating scale changes in trials that are powered to ensure that clinically insignificant changes achieve statistical significance. It would be entirely possible to prove Snake Oil was effective on this basis.
Meanwhile in the real world
Meanwhile in the real world, there are in fact more dead bodies in the active treatment arms of most blockbuster studies than in the placebo arms. The claim that these surrogate or rating scale changes demonstrate effectiveness therefore as a matter of logic does not stack up.
Aside from dead bodies,we know that many of those who “benefit” will have enduring problems from physical dependence and other legacy effects from treatment. This is not effectiveness as the 1962 regulations envisaged. We have ended up instead in a world in which hints of an effect are used to gain market entry for drugs and when we use these drugs mindlessly on the basis that they are effective, if the RCT evidence is to be believed, we produce greater disability in the long run than if we never had them. The effects may turn out to be worse than if we had encouraged chronic alcohol intake.
The only thing that stands in the way of this outcome at the moment are the dwindling number of doctors who pay no heed to guidelines and try to be discriminating in their prescribing and the patients who simply don’t take the treatments when their experience tells them this is not for them.
Trial perversities
So far the argument is consistent with a view that controlled trials are gold standard processors into which we have fed garbage and have got garbage back. And that many people have a great capacity to greet garbage as gold.
In fact, we are cursed like Midas and everything to do with this gold standard, rating scales and surrogate markers, has produced an informational reductionism and rigid standardisation that is destroying medical care.
Little noticed is the fact that the RCT processor malfunctions badly in a number of ways.
Whenever a drug and an illness produce superficially similar effects from pain, to nausea, to suicide, it is possible to hide drug-induced problems. Antidepressant trials can be “gamed” so that drugs known to cause suicide will show up as preventing suicide rather than causing it. Perverse outcomes like this are built into RCTs (See The Best Bias that Money can buy, Heads we win, tails you lose).
In all these cases, the Christmas tree lightbulb test is better than clinical trials ever could be. When the lightbulbs don’t work after they have been laid up for a year, you unscrew each in turn, till unscrewing one leads the lights to come on, screwing it back in causes them to go off again and removing it turns them on. In this case, we have as definitive a result as Martin Teicher had with Prozac and suicide in 1990. Lilly claimed their clinical trials showed no problem. Teicher’s observations can now clearly be seen to be much more valid than Lilly’s.
When we get clearcut results from celebrated trials such as the Women’s Health Initiative study of HRT, it’s often because these are conducted in essentially healthy volunteers so that excess rates of breast cancer stand out – this was a drug trial rather than a condition trial.
Confused outcomes also happen when the clinical condition being investigated is heterogeneous as for instance in back pain, depression or asthmatic states or even Parkinsonian syndromes. In the case of SSRIs and suicide, GSK were able to use the different background rates of suicidal acts in borderline personality disorder patients compared to major depressive disorder patients to hide the suicide risk on paroxetine. The same can be done on purpose or by accident for many if not most medical conditions.
Finally in the case of the antidepressants, although in Lou Lasagna’s hands imipramine didn’t beat placebo, it is relatively straightforward to design trials to get imipramine to beat SSRIs – all that is needed is to pick a group of more severely depressed patients. But in this case, what would FDA license imipramine for? For severe depression only or for all depressions and what consequence if any would there be for the licensing of SSRIs?
Panalba & combination treatments
It was the issue of relative efficacy that blew Lasagna’s career off track in the fiercely contentious Panalba case in 1969.
Panalba, as mentioned (see Tragedy) was a combination antibiotic. FDA wanted to pull it off the market – on the basis of efficacy not safety. They claimed that the test of effectiveness for a combination antibiotic was a demonstration of effectiveness over and above the effectiveness of each of the individual components.
If we compare the regulation of drugs with the regulation of butter, FDA never takes a position on the comparative merits of butters. In similar fashion, FDA does not now allow, and likely never will allow, comparative effectiveness claims to stand within a therapeutic domain.
But in the case of combination antibiotics, FDA chose to remove all such treatments. Lasagna publicly contested the issue, not as a believer in Panalba, but on the point that the basis for the decision appeared arbitrary. He argued it was bad medicine to use Panalba. But was it up to Medicine or up to the FDA to sort this out? And, although philosophically against Panalba, he wasn’t prepared to completely deny some place for clinical wisdom in its use.
Panalba was an obvious combination drug. But many drugs embody several therapeutic principles – they are cocktail drugs rather than combination drugs. Imipramine contains an alerting norepinephrine principle, an anxiolytic serotonergic principle, a euphoriant anticholinergic principle and a sedating anti-histaminic principle. In just the same way some antibiotics embody more than one antibiotic principle. Indeed Prozac has antibiotic effects. When it comes to the licensing of cocktail compounds like this, FDA does not and cannot require a demonstration of greater effectiveness.
In fact a good case can be made that it is imipramine’s cocktail nature that makes it difficult to run an RCT on it. It has an anxiolytic effect, but not so marked as Prozac, an alerting effect but not so marked as a stimulant, and a sedative effect but not so marked as an hypnotic. This cannot be brought out in milder depressions but imipramine is clearly better than Prozac in severe depressions and in clinical practice a discriminating clinician can deploy its many facets to good advantage, regardless of what a purist might prefer. Good practice with this drug and many other drugs will never be RCT based.
If so for imipramine, to return to Lasagna’s point, what about Panalba? Imipramine is just one drug – but FDA have since licensed many combination treatments from Fen-Phen to Symbyax (Prozac and Zyprexa) none of which met 1969 standards for efficacy.
Compromising safety
When it comes to safety the problems get more acute. The effectiveness requirement is enshrined in regulation for the contribution it makes to safety. If all drugs are poisons then there is a better risk-benefit trade off if we have some confidence there is a potential benefit to trade against. The wording of the regulations continues to put safety first – safety and effectiveness.
But in using RCTs to demonstrate effectiveness Congress compromised safety. Here’s how. RCTs necessarily have a primary endpoint for purposes of calculating statistical significance. The assessment instruments and trial design hinge on getting the best possible data on the primary endpoint – which is always the demonstration of effectiveness. This focus on one endpoint means that other outcomes (safety issues) are side-lined.
As a result, if in the course of a study a safety problem happens at a greater rate on drug than on placebo, it will be poorly characterized, will be hidden under multiple codes and will almost always be dismissed as not statistically significant – even by FDA. Under oath, Andrew Witty will swear we had no evidence that our drug caused this problem, and he may not be lying in the conventional sense of that word.
The 1938 act FDA clearly took effectiveness into account. It used to be impossible to discuss safety without efficacy. For example, the early sulfonilamide drugs were dangerous but in view of their effectiveness in saving lives, there was little question but that they should be allowed on the market. A hypnotic shouldn’t cause birth defects or peripheral neuralgia and under the 1938 Act, thalidomide wasn’t licensed.
But under the 1962 Act, the claim that effectiveness has been demonstrated now means that some of the most problematic drugs in medicine, such as dopamine agonists like ropinirole that cause gambling, sex addiction and personality change, can be brought on the market for conditions like restless legs syndrome. Common sense doesn’t seem to apply any more.
As a means to promote safety, the effectiveness criterion fails. This might be acceptable if the criterion ensured we got effective treatments but comes close to lunacy if the drugs are not in fact effective, and is even more lunatic if doctors can be brainwashed into thinking they are effective.
Is the effectiveness criterion unconstitutional?
In July 2012, GlaxoSmithKline paid a record $3 billion fine for off-label promotion of several of their drugs. A few months later, and they might not have had to pay anything.
In December 2012, in the Caronia case a Second Circuit court ruled that stopping a company representative from talking about off-label uses of the company’s drug was a breach of their First Amendment rights to free speech. There was consternation among supporters of regulation.
The case involved Alfred Caronia, then a sales representative for Orphan Medical, which sold Xyrem, a drug approved for narcolepsy. He had been caught on tape discussing the use of the drug as a treatment for insomnia, fibromyalgia and other conditions with a doctor who was a government informant. He was convicted in 2008 but appealed on the basis of the First Amendment.
Since 1962, companies have for the most part supposedly demonstrated drug A is effective for condition X in order to get a license. They are then restricted to promoting the use of A for X, while doctors can use A for anything. It is more rational for instance to use SSRIs for premature ejaculation than for depression, as SSRIs are extraordinarily efficacious for this. But if a company representative suggested such a use when his company had not applied for a license to market the drug for this purpose, the company could be penalized.
The ruling in Caronia stated:
“The government clearly prosecuted Caronia for his words — for his speech,” but “the government cannot prosecute pharmaceutical manufacturers and their representatives under the FDCA for speech promoting the lawful, off-label use of an FDA-approved drug.”
Judge Debra Ann Livingston disagreed, arguing that
“[this] calls into question the very foundations of our century-old system of drug regulation.”
In a statement to send a shiver up the spine of most “liberals”, the Pharmaceutical Manufacturers Association said:
“PhRMA believes that truthful and nonmisleading communication between biopharmaceutical companies and health care professionals is good for patients, because it facilitates the exchange of up-to-date and scientifically accurate information about new treatments.”
Whatever about politics and preferences, it’s intellectually difficult not to side with the judges and PhRMA here. As things stand, anyone on the planet can discuss off-label uses of most drugs except the company that has made them. Worse again, when it comes to other drugs it makes no sense to say a company could only talk about the use of an opiate analgesic for gall-bladder but not for lung cancer surgery. This is an artificial debate created by the effectiveness criterion.
Just as with drugs, Olive Oil has to meet a regulatory criterion to be let on the market. The criterion doesn’t specify use of Olive Oil as a salad dressing as opposed to its use as a cooking oil. If the criteria did specify this, once on the market, if it was discovered that Olive Oil was wonderful for massage purposes, it would clearly be an infringement of the right to free speech to stop a company representative talking about these benefits, especially of Extra Virgin Olive Oil.
The Pied Piper
So what had Michael Shepherd said in his lecture on The Placebo that reduced an American audience to silence?
At dinner after the symposium in New York, Lasagna told Shepherd the placebo had been completely eclipsed within American medicine. No-one had any idea what it meant – and no-one was likely to grasp the issues he had raised.
What Shepherd told his audience was that bizarrely the awareness most doctors have of placebos stems from controlled trials. But the RCT placebo has almost nothing to do with the Powerful Placebo of the 1950s. It’s a stochastic effect. It’s meaningless. In any particular trial no-one knows or can know whether it refers more to the biases of doctors or of patients or to the natural variability in the condition.
When it comes to treating an individual patient or evaluating what is likely to be going on, the fact that there is a placebo response in population studies of medical conditions tells us next nothing.
The placebo response in controlled studies looking for an effect on a structure or function of the body would be quite a different matter and is something that could be usefully explored for learning or other effects that might in their own right form a basis for other or additional therapies. Just as placebos in testing for analgesia can show profound conditioning and other effects, so too they could in testing for anxiolysis for SSRIs. In depression studies the role of the drug and placebo tell us nothing other than a regulator can possibly approve this drug. It’s almost anti-evidence based medicine.
Lasagna and Shepherd were at one on this. As Lasagna put it:
“Evidence Based Medicine has become synonymous with randomized placebo-controlled clinical trials even though such trials invariably fail to tell the physician what he or she wants to know which is which drug is best for Mr Jones or Ms Smith – not what happens to a non-existent average person”.
He went further, noting that all drug discovery in psychopharmacology had been made by men like Fritz Freyhan who had been so skeptical of clinical trials in 1956 (Empire of Humbug 1), rather than through trials:
“The days when a drug company would go to skilled and sophisticated psychiatrists and give them a supply of a new drug and ask them to try it on some different patients seem gone forever. Is this a cause for celebration or depression?”
When asked in 1996 about the developing “craze” for Evidence Based Medicine, Shepherd responded that if we went down this route:
“We would also, of course, never make any advances because all advances depend on guesses which we call hypotheses – most of which are wrong but some of which are right. In terms of the logic of the scientific process the evidence comes after the hypothesis. You must begin with a hypothesis and that is a guess.
I knew Cochrane but [Evidence Based Medicine] is pushing the thing to, I think, an absurd extreme. Of course, it’s true that the whole discipline is cluttered up with procedures for which the evidence is meagre at best and there is a case for trying to make quite certain that that is minimised. If that’s what meant by it – certainly – but it eventually stiffles everything else”.
In fact where the placebo had once seemed a form of hypnosis, the focus on effectiveness and specificity has turned RCTs into a form of hypnosis. Doctors are now in thrall to the spell of the hypnotist from Oz, who’s RCTs can even make Snake Oil to be effective.
Hypnotized by the Piper’s tune, doctors and patients are lured to consume 6, 8 or 10 drugs at the same time – what could be wrong with taking drugs that work. Infants, elders are lined up and medicated. The only ones who may be saved are those who have been previously crippled or injured on whom the music has ceased to work. Few can see what is going on around them or the name of the theatre in which they are being duped – The Empire of Humbug.
At long last, in this series of posts, we have someone who does both clinical and research medicine and who is prepared to say, loud and clear, what the limitations of the RCT are. Furthermore, David is telling us what the implications of the current infatuation for this tool have for the future of medicine.
So far, I think I have listed from David’s posts, the following consequences of over-use of the RCT as follows (in no particular order):
1. Failure to discover and record adverse events adequately.
2. Intrinsic weaknesses in their formal approach which allows “gaming” by those with a vested interest in the outcome.
3. A restraining or even blocking influence on future research for new possibilities; partly by the gobbling up of financial resources and partly by the inversion of hypothesis driven research.
4. Failure to tell the clinician what they actually want to know.
These are all things which Goldacre does not point out in his book, but rather, goes on to advocate more of the same. His publicity machine is so efficient, and the hype so loud and ubiquitous, that it is begining to look as if the medical professions are going to render themselves redundant in favour of menu-driven software to diagnose and treat the patient.
I have forgotten:
5. What David calls “disease mongering” which (I think) is the search for any significant result emerging from multiple outcomes (often proxies for real conditions) and the marketing of a drug on the basis of having found significance. There is a tendency to do something similar by the description of “new diseases”, giving them new names and then finding a drug which will treat this new disease, but I suspect this latter practice is less prevalent than the variant David has highlighted.
http://www.parliamentlive.tv/Main/Player.aspx?meetingId=13017#
Who were those seedy men from GSK and Roche and what was that woman from the EMA talking about. Is she blind to trials transparency prior to 2004 and why is she saying it is all so complicated.
It is not complicated at all.
It is easy, if they all get their heads out of the sand.
One point to Ben, zero for the committee…..
Do any of these people actually consider lives lost, or is this ongoing committee talk destined to allow GSK and Roche spokespersons to sit in their high office of corruption and sit in these sorts of committees and give out their usual talk the talk and not give a damn about lives lost.
Even Ben, with his tough talk, forgets about lives lost……..
Back to the drawing board…..
These sort of meetings where they all talk the talk is so crass, that I do not wonder that, us, at the bottom end of their talk are left in sheer bewildering bafflement that talk like this is uttered……
Congratulations to Professor Healy for a goodly article in the Mail Today about Rxisk. Well done, Jerome Burne, and Anne-Marie for just a little bit about us….
Committees. Good try. Fail. No-one came out of that particular meeting very well.
Thank you for this.
Just as some feed-back from a reader, I would find it helpful to have links/citations for some of the claims being made, (although I realise this can make blogging more work). I’m not familiar with a lot of the issues being discussed, so it can be difficult to know where to start with some of the claims, so if you do have links easily available when you’re typing something up, I’d vote for you including them!
Also, while I need to read more of your earlier blogs (I have read some), I’m not sure why there’s any necessary problem with RCTs. RCTs can be spun and manipulated, and it’s foolish to think that just because results are from and RCT they can be trusted… but RCTs should allow for sub-grouping, etc to find out which drug is likely to be best for Mr Jones. Is the argument that the cost of doing RCTs well is such that they tend to be done by those with the money to do them and a financial incentive for a certain result? If one had access to sufficient funding for an RCT, I do not see how this could be less useful than any other way of testing a treatment. I don’t see how the justified criticism of RCTs leads to the implication that there are better ways of testing treatments. Thanks.
RCTs are a good way of casting doubt on claims a treatment is effective. If there is an overlap between an effect of treatment good or bad and an the effects of the illness, then RCTs are not a good way to work out whether the drug has benefitted or harmed particular individuals – that is much more likely to come from N of 1 trials
Ta.
So the limitations of RCTs and our understanding as to how to meaningfully sub-group patients are such that RCTs showing that the best treatment for patients with the characteristics X, Y, Z should not allow confidence that the treatment is helpful for a patient with characteristics X, Y, Z. The use of the treatment should be seen as a cautious trial.
(I may have imposed my own thinking on what you said there). In a lot of ways, this sort of medical scepticism and caution about would seem likely to lead to quite a dramatic change in the traditional relationship between doctor and patient. It sounds like it would be an improvement. Thank you.
We have known for a long time that imipramine and some older antidepressants are good treatments for melancholia. We don’t know this from RCTs – we know it from clinical experience. In RCTs imipramine often fails to beat placebo if given to a group of patients united only by having depressive symptoms. You could go back and do an RCT in melancholia and then it would beat placebo easily (SSRIs wouldn’t). But companies would never do this because this would likely restrict their market.
Having said all this, imipramine has a number of therapeutic principles in it and a good doctor can put these to good use in a variety of patients – bearing in mind the risks of agitation and suicide, dependence and withdrawal that come with it
I see, ta. While I appreciate your criticisms of RCTs and the trust some place in them, I have even less faith in clinical experience as a guide to treatment. There is a serious problem with money and power skewing medical research (and other areas of research too!), but couldn’t those clinicians who believe imipramine is a preferable treatment for melancholia perform some sort of RCT of their own? I realise that there are limitations on what can be done with limited funding and time, but honestly done RCTs do have many advantages over a series of N of 1 trials. There is a long history of ineffective treatments being supported on the basis of clinical experience, and so many potential biases which can effect people’s perceptions of results, so I think RCTs are still the best of a bad lot. Thanks.
Well here’s a question then. RCTs of beta-blockers will unquestionably show that these drugs slow heart rate. If i put you on a beta-blocker and your heart rate goes up dramatically. What would you want me to believe – the RCT evidence or the evidence of our joint pairs of eyes? The useful role of RCTs is to eliminate from the market treatments that don’t work but they are now being used to all but forcibly medicate people with treatments that don’t work for them.
I’d certainly agree that some have come to place too much faith in the results from RCTs, and that doing so can be harmful to patients. We should not assume that, because RCTs show that a drug tends to have a certain effect, it will do so in all individual patients, so should be cautious and wary of side-effects, like beta blockers potentially increasing some patient’s blood pressure. However, even if a doctor were to have a series of patients for whom beta-blockers did serve to increase blood pressure, then this clinical experience does not mean that they should believe beta-blockers are a drug which tends to increase patient’s blood pressure!
I’m not currently confident that RCTs are even able to eliminate from the market treatments which do not work, particularly for talking/cognitive/behavioural treatments where blinding is difficult and control groups often inappropriate. In unblinded trials with an inappropriate control, homeopathy can be shown to improve self-reported symptoms – I don’t think that this shows it to be effective in any meaningful sense. Also, RCTs should, if enough of the right sort of information is gathered and they are done honestly, be able to help test for sub-groups of patients who respond in different ways (although this is also open to abuse), as well as providing information about the levels of improvement that tend to follow different interventions. While the problems with RCTs and the environment in which medical research takes place are currently such that I think it is best to remain cautious and sceptical about the results being presented from RCTs, if I was to conduct research examining the efficacy of particular treatments, I would want to run an RCT. Thanks.
There are two points here – one is testing for efficacy – where RCTS are often not needed. In testing for effectiveness they are needed and are mainly helpful when they exclude ineffective treatment. When treating you the evidence of your and my eyes sd be paramount – supplemented but not replaced by a belief system drawn from good studies which give us some grounds to believe that doing what we are doing might be helpful. Studies here can include but does not mean RCTs. Pretty well 100% of new treatments are discovered because of studies that are not RCTs.
I agree about the limited use of RCTs and the danger of a misguided faith in the results presented from them, but I’m afraid that I still don’t understand why non-RCTs would be seen as a preferable way of gathering data. re the imipramine for melancholia example, I don’t see why a series of N = 1 trials would be preferable to an appropriately designed RCT. Is it just that the added cost of RCT’s means that only certain interest groups tend to be able to perform them? Other than that, RCTs seem a good way of accounting for certain biases. Sorry if I’m missing your point here. Ta.
RCTs derive from agriculture. They account for the biases that might come into play with fertilizers. The biases of sunlight and drainage etc. But if both the drug and disease can produce the same thing – either a benefit or a harm – RCTs are lost. And when in fact I treat you how are we going to tell whether what is happening to you is good or not – do we go by the Evidence base and say well the evidence shows the drug works and has no harms therefore even if it doesn’t look like you’re getting better you must be?
I agree that some can place too much faith in RCTs, and that patients and doctors should be committed to looking for evidence that an individual patient is not responding to treatment in the way which data from RCTs indicated that they would be likely to, but don’t see how this leads to the belief that a series of N= 1 trials are preferable to an RCT. When the symptoms of an illness and possible side effects can overlap, working out which is which is difficult, but randomisation and the use of an appropriate control group is still surely useful.
While I agree with your specific claims about the problems with RCTs and the way in which they are viewed, I don’t see why this leads you to believe that non-RCTs are preferable. I’ve thought about ways of assessing the value of imipramine as a treatment for melancholia, and haven’t been able to think of a reason why an RCT would be less useful than a series of N=1 trials. Ta.
The Caronia case you mention is a complicated one, but to me the issues seem awfully similar to the lamentable Citizens United case allowing corporations unrestricted campaign spending in the name of “free speech.” Are corporations people, and is money speech? A growing majority of us say no – if millions of dollars from anonymous private interests can drown out the voices of local voters, it brings us way too close to a system of one dollar, one vote.
The Caronia decision goes farther in expanding freedom of commercial speech to corporations marketing a potentially hazardous product: In order to sanction any claim they push, the burden is on the state to “prove” the claim is false. Even if we had a government agency with the money, power and motivation, how could that be done? To a 95% certainty? In a randomized trial? Short of that, if the corporation has one “peer reviewed” journal article to stand on, they could be home free. And if the FDA has no power to limit Pharma’s claims, forget about the unions and consumer groups who have sued them for fraud in recent years. Most of those suits, which have at least rocked the boat and publicized the abuses, will now be thrown out of court on the first bounce.
I’m not terribly worried about what a guy like Caronia says to doctors. As you have pointed out, the drug companies have learned to co-opt and use medical “key opinion leaders” to become far more effective drug reps than the drug reps could ever be. But I do worry – big time – about the “speech” Caronia’s bosses could be allowed to flood the airwaves with through virtually unregulated direct-to-consumer advertising. (Worse yet the Internet, where they can directly target the eyeballs of those seeking help, and purchase the first forty places on any Google search so that no other voice gets through.) How this decision would affect DTC ads is still hotly debated, but this Supreme Court has delivered for business beyond even business’ wildest dreams. So may as well prepare for the worst.
I have to admit, the current patchwork regulatory system is pretty pathetic and lacks a certain intellectual consistency. That’s not to say it can’t get much worse. No doubt GSK would say that its lack of DTC advertising in most of the world including Britain is a violation of “free speech.” Should they get their “rights” worldwide, then?
Johanna
As ever you have framed the issues perfectly. We need to prepare for the worst. The next two posts in the sequence are about preparing for the worst.
Healy, I enjoy your articles very much. This world would be a million times better if every psychiatrist were as critical of drug companies as you are. We all need to be critical of drug companies and their meds. Here in the U.S. half the country puts our president under such scrutiny because he has the ability to control our lives in certain indirect ways, but many of these same people will take a psychiatric med and all they care to look at is the side effects sheet that comes with it and they’re satisfied this way. They will defend these meds to the very end on a forum I get on. Some even are supportive of not letting patients know of certain side effects so that they’ll be more likely to take these meds.
Anyway, I’ve been curious about your stance on Electro Convulsive Therapy? What do you think about this treatment?
Specifically I’m wondering if you think ECT can have permanent effects such as messing up someones memory or cognition?
Micahel – its not my role to tell you or anyone what you should or shouldn’t have. Have never wanted anything banned. The key issue if you and i are working as a team is that we have a full set of information available to us – which we don’t have for any drug and in this sense it is difficult to do pharmacotherapy with informed consent.
When it comes to ECT there are lots of people who want it and others who would never have it. I would want it available for those who find it helpful and would champion the rights of those who do not want it to avoid having it.
Regarding what to tell them re memory it would be something like this. When you get to the stage of contemplating ECT you almost certainly have had a bunch of treatments that affect memory. Benzodiazepines have very clear effects on autobiographical memory. Antipsychotics and mood-stabilizers have clear effects on set shifing – being able to remember someone’s phone number. ECT also certainly has effects on memory also but its hard to know precisely what. I have had people tell me about their memory problems post-ECT and describe very clearly memory problems of the type antipsychotics cause which they blame on ECT even though they are taking antipsychotics.
Overall far more memory problems are caused by drugs than ECT and vastly more people are on involuntary drug treatment than involuntary ECT – so if there is an issue to campaign about it should be the drugs
Which would you choose ssris or benzos, is the question.
Definitely benzos because, on the whole, in my experience, there is so much publicity about benzos being highly addictive, that the message has more or less got through to some doctors.
Ssris are a different kettle of fish entirely.
Although having similar withdrawal, the million dollar dilemma for doctors is that they know nothing about ssris, nothing at all, and so ssris become so dangerous, so macabre in their oft sudden withdrawal that all hell breaks loose, whereas with benzos, the acute withdrawal is bad, but not so very bad.
Depends on your definition of bad…..
I have experienced both.
I received copious quantities of benzos, valium, ativan, for much longer than the recommended time of two weeks to combat ssri abrupt withdrawal.
So, not only was I was going through abrupt ssri withdrawal, but I was, then abruptedly left to my own devices, abuptedly off valium and ativan, as well.
I would also add that valium and ativan did not do anything to help with abrupt ssri withdrawal. This was so terrible that even copious quantities of valium and ativan did not penetrate the withdrawal from the ssri.
So, all in all, a rum do.
I would have preferred, maybe, a two week course of a benzo, not two years of Seroxat and then plummeting to dangerous depths…….and then handed out benzos like smarties.
People who mis-manage drugs like this, to an ordinary every day person, are a total danger to society and although, I, know better, now, and managed to come out the other end, this was largely due to pure ignorance on my part.
The more you learn the scarier it is for the pill popper, who looks at the doctor with a new attitude of pure, unadulterated despair and desperation and, dare I say it, despise….I could now become an excellent gp as I now understand so much about it.
I have empathy and compassion and I am sure I could work out a ‘pill plan’ not a botched and barbaric Plan B, for benzo, which was a hopeless state of affairs.
Moreso, when patient is ‘piggy in the middle’, as I was with two opposing and different tactics, both of which failed miserably because ‘two’ failed to talk to each other and they were only a pretty, half hour drive from each other…
I was the tennis ball ricocheting between them. Clueless doctoring.
Benzos, without the added ssri complication, have their place.
Ssris have yet to find their place amongst all the confusion of where to put this class of drugs in the great scheme of things pertaining to drugs helpful or drugs unhelpful…….
Hope that was helpful.