
Continuing the Spotlight on the Suicides Series
I have largely avoided naming names and will continue to avoid putting names in the frame but Stephen’s family doctor’s name, Dr Brannigan, is already in the public domain, and I’ve made it clear that the coroner thought highly of him and the whole point behind these posts is to show how even a decent doctor can end up in a nightmare. These posts are about a rotten barrel not a rotten apple.
Dr Brannigan had his own lawyer present. The hospital had theirs.
He seemed a decent man. There was a longstanding relationship between him and the family. Stephen had been his patient for years and the two appeared to get on in a manly way.
He began nervously.
Prozac & CBT
Some years before, Dr Brannigan had spoken to Stephen when he was grieving after the death of a parent. This conversation led to a prescription for Prozac. The script was repeated once.
Prozac clearly didn’t work and Stephen may not have taken much of the first course. But like most of us, he took the second script from his doctor – finding it difficult to tell him he’d stopped taking the tablets.
How do I know this? We know 50% of people stop the SSRI they have been given within a month because it doesn’t suit them or they feel its not really needed. Stephen’s family mentioned he hadn’t thought it suited him and had stopped it. Dr Brannigan didn’t renew it after the second script, which he would have done had either he or Stephen thought it been working.
After the second script, Stephen according to Dr Brannigan was better and didn’t need any more. When pushed on whether he thought the drug had made him better, he declined to say it had helped.
There was no entry in the record saying it had or hadn’t helped. For lawyers who have no idea what giving an antidepressant means, however, the lack of an entry saying it hadn’t helped meant there was no evidence it hadn’t helped or caused problems in any way.
Some time later, when Stephen was out of sorts Dr Brannigan suggested a course of CBT – rather than more Prozac. Stephen agreed but again gave this up after a few sessions. He was a get on with life person rather than someone who liked to pick over things.
Enter Doxycycline
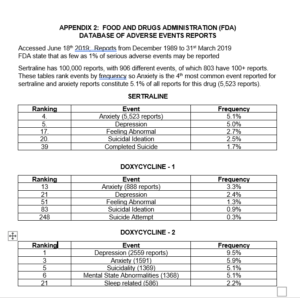
In early 2016, Stephen had a chest infection that didn’t respond to the first antibiotic he was given. One of Dr Brannigan’s colleagues gave him a prescription for a week’s doxycycline. The chest infection cleared but almost immediately afterwards Stephen complained of anxiety. The table here replicates last week’s table – Spotlight on the Coroner
The first point to note is Doxycycline is among other things an SSRI. Dr Brannigan was not to know this – very few doctors do. But you don’t need to know how a drug works to know what it’s doing. You just have to listen to and believe the people who have taken it when they tell you what’s happened to them since they took it.
Doxycycline is well known to cause suicide in people who have been given it for acne or malaria prophylaxis or for chest infections. Only marginally less likely to cause suicide than isotretinoin (Accutane) when given for acne.
Second, the comparison of the two doxycyline sets of figures in the Table above brings out how FDA reports can hide problems. In addition to reports of depression, there are reports for malaise, asthenia, depressed mood, anhedonia and mood swings, all of which added up make nearly 10% of the reports on doxycycline – even without adding in reports of emotional disturbance, emotional disorder or other events that could conceivably have been depressive.
There are similarly separate reports for anxiety, agitation, panic attack, nervousness, fear, restlessness and stress. All told over 25% of the reports on this drug are related to suicide or its antecedents.
If you apply the same logic to sertraline, quetiapine, mirtazapine and buspirone that featured in Appendix 1 in last weeks post – the one page of data the coroner decided not to admit as evidence – you can guess what the true profile of the effects of these drugs is likely to be.
In response to Stephen’s anxiety, with no sense it was caused by doxycycline, Dr Brannigan referred Stephen for counselling. Counselling, CBT, Mindfulness or whatever are only likely to make a problem like doxycycline induced anxiety worse – as the therapist tries to persuade someone their real problems stem from being bullied at school or whatever. Fortunately or unfortunately, the waiting list for therapy was long.
Another point to note is that this adverse response to a serotonin reuptake inhibitor fits the profile of a poor response to Prozac – another serotonin reuptake inhibitor and antibiotic as it turns out. In a situation like this, it can be expected that the next serotonin reuptake inhibitor will produce an even worse response.
While waiting for counselling, one day when Stephen came into the surgery, Dr Brannigan decided to give him sertraline. On the witness stand, he made out that Stephen seemed totally different to the usual Stephen and he Dr Brannigan figured this was more like a real depression than the rather minor nervousness that had led him to prescribe Prozac some years before.
At least this is what he said on the stand at the inquest. The medical record doesn’t bear this out.
This account is not accepted by Stephen’s family. Nor is it consistent with his activities at the time that show him continuing to do things such as play in concerts. They knew he was out of sorts but didn’t notice a dramatic change at this point in time.
Why sertraline? Well according to Dr Brannigan there is evidence that this is better for dealing with proper depression. There isn’t. The sertraline literature is comprehensively fake. Any hints that it is better for a severe depression is pure marketing copy.
More to the point, whatever change there might have been in Stephen that day paled in comparison to what came next. Up to the evening he took his first sertraline tablet, Stephen O’Neill was a man who had had no contact with the mental health services and neither he nor his family ever envisaged him having contact.
After he took his first pill, for the remaining 6 weeks of his life he was in constant contact with the services and pretty well every moment of contact made things worse.
Serotonin Pick-up Syndrome
After a catastrophic response to sertraline, Stephen ended up in hospital briefly. The medical notes are clear – he told people that sertraline had caused all his problems. This was noted but not heeded.
There he was given lorazepam in a low dose one evening just before discharge and found it tremendously helpful. His view that it had close to normalised him was recorded in the medical record.
When he returned to Dr Brannigan, the lorazepam was not continued and Quetiapine was introduced instead. This as a previous post has noted made things worse. But although Stephen reported being worse, the Quetiapine was not switched back to a benzodiazepine.
Why?
This is because pharmaceutical companies did an extraordinary hatchet job on the benzodiazepines in the 1990s as part of the marketing of sertraline, paroxetine and fluoxeting (Prozac). Most family doctors in the UK ended up quite literally thinking the benzodiazepines are more dangerous than opioids and that in comparison SSRIs are harmless. They still think this and dish out opioids more liberally than benzodiazepines.
This reputation continues to this day, when prescriptions for benzodiazepines are a fraction of the scripts for SSRIs – with over 10% of the population hooked to an antidepressant. This reputation persists even though within 3 years of its launch in the UK, there were more reports to the UK regulator of dependence on paroxetine alone than there been in the previous 20 years for all benzodiazepines combined.
This is the case even though when marketing SSRIs in the 1990s, the companies went around telling family docs that in the early phase of treatment with an SSRI there could be a serotonin pickup problem but not to worry this would pass and it could be managed by giving their patients diazepam or lorazepam to take during the first few days of treatment.
The point here is not that benzodiazepines are safe, although I, and I’d imagine most people working in the secondary mental health services, if given a choice between diazepam to take everyday for a year or fluoxetine or sertraline would take diazepam. The point is that Stephen was handing Dr Brannigan and everyone else who was in contact with him the diagnosis on a plate.
It could not have been more clear. And he could not have been more ignored. He was ignored by decent and even good people – in much the way that people abused by the clergy in the Catholic Church were ignored by decent and good bishops or other clergy.
This ignoring is a public health hazard. Inquests are supposed to be about trying to minimise risks to the public health.
Next Week: Spotlight on The Hospital Doctor
A snippet from From justice.gov.uk/courts procedures It’s worth reading the whole thing – there seem to be plenty of loopholes to crawl through
It seems as though the transcript was given but not put online? It’s confusing if a case can be closed without goinf through legal procedures. Especially as this case is described as a model to used in other cases. The coroner is also someone who gives seminars to the Law Society so his judgement about this muddle being a model is ridiculous.
(ii)
25.19
(1) Within 10 business days after the final hearing, the party who instructed the expert or, in the case of a single joint expert, the party who was responsible for instructing the expert, must inform the expert in writing about the court’s determination and the use made by the court of the expert’s evidence.
(2) Unless the court directs otherwise, the party who instructed the expert or, in the case of the single joint expert, the party who was responsible for instructing the expert, must send to the expert a copy of the court’s final order, any transcript or written record of the court’s decision, and its reasons for reaching its decision, within 10 business days from the date when the party received the order and any such transcript or recording
So sad that the obvious is not acknowledged.
Also later the same day after reading this I read this
https://www.rnz.co.nz/news/national/402858/more-young-new-zealanders-using-antidepressants
It is sickening what is happening. Schools are now pushing mental health blah blah blah see a doctor blah blah blah get help blah blah blah. We all know the fate that awaits and its tragic. True story…..recently got talking to a parent of a high school student year 11. When she quietly told me her son was adhd my bullshit antennas suddenly came to life. I quietly asked how did this diagnosis come about. Wait for it…she told me some people came to her sons school to talk about mental health and symptoms etc. Her son came home and told her after listening to this he thought he might be adhd. So off to the psychiatrist they went and sure enough surprise surprise (not) he was diagnosed adhd. I then said he’s not taking drugs for this is he. His mother replied yes he’s been taking Ritalin for a year now!!
Once again proof that if anyone thinks they have a mental diagnosis they will have no trouble finding a doctor to agree with them…no clinical assessment required.
Watch this space nz’s Suicide rate will only continue to skyrocket due to this criminal ‘rotten barrel ‘ situation.
Getting in to the, ‘Doctor’s’ head..
It doesn’t disappoint..
The Doctor’s head is a strange place; they make pronouncements which are clearly untrue, they talk about ‘medication’ as if they were an expert, when they clearly don’t know what they are talking about, they pick-and-mix without the least understanding of how they are bouncing around the recipient.
You would think that Stephen would be luckier than most, his doctor having known him for some time. How Stephen was before taking the drugs and how he then became.
But, apparently, not.
I hardly think we need to spell out that most doctors are pretty oblivious about the true nature of these drugs. Switching the Lorazepam to Quetiapine, was pure madness.
Why do doctors not understand, most of which is written here.
They don’t listen to their patient, they make up extraordinary and unbelievable reasons for taking the actions they do, they become defensive, when charged, they don’t seem to understand people and they don’t seem to understand how collections of drugs, seemingly, chosen at random, can and do render the patient an insignificant body who is thrown in to extremes and who now inhabits, No Man’s Land.
In so many ways I can relate to what Stephen went through.
If my gp had called an ambulance, instead of telling me to drive myself to a mental hospital.
If the mental hospital consultant who had prescribed Seroxat, had continued to give me the diazepam to take home with me, thus potentially, avoiding, an ambulance visit to a main-stream hospital..
If.If.If..
I advised my girlfriend not to take the Sertraline; her Doxycycline was poking out of her bag another time. I was given Doxycycline a while ago, and I said to the doctor, don’t ever give me that drug again. Oh, did you have a hard-time, he said. Brutal.
Bearing in mind, Stephen is dead, I can completely understand why his doctor was nervous, and had a lawyer – not a nice thing to have on your conscience, if you have a conscience …
Any evidence of ‘Informed Consent’ in the notes? Well m’lord we did explain it to him, verbally, and he understood all the potential for causing harm including suicidal thoughts. Seems the notes werent ‘doctored’ or ‘missing’ or ‘lost’ this time Were they computerised? which makes that possibility harder these days. Instead of getting around together to settle this horror and apologise and call for better training especially the need for access to expert knowledge about drugs – they especially the family doctor compound it by betraying Stephen O and his family. Forgive them they know not what they do? No way ,they knew sod all about drugs, practiced ‘beyond their competence’ and then looks like colluded together. Wonder what the blah blah from the General medical council would be after another few years on the merrygoround.
I don’t think progress will be made unless people are named – but the family doctor will be used as the fall guy by the lot of them unless the others are named too.
Drs don’t want people to die because of their mistakes. I worked in a hospital and to be honest I saw all the drs go above and beyond to help their patients. They worked long hard hours and you could see the anxiety and tension in them when they had a problematic patient to deal with. I knew from what I witnessed Drs really do have your best interests at heart, they really don’t want to harm you. What I didn’t expect to see though was when and if something did go wrong they would club together to conceal the mistake and make sure they weren’t blamed.
When I say mistake I mean mistake because I don’t believe any Dr wants to deliberately hurt or harm you but on the small occasions it happens and unless it’s an outright neglect or deliberate harm they will cover it up in anyway they can to prevent any one person being blamed who was otherwise an excellent Dr who had saved many lives before.
Drs do mean the best for us but it’s the system maybe that is turning Drs against us. It’s the system we need to confront. Drs should be able to without fear report suspected side effects without fear of persecution.
Could this be were the problem lies.
Agreed. Most physicians do not want to do harm. There are many good physicians however, there are many physicians both good and bad, who do not listen to patients in part at times or in whole. There is this hubris if you will and honestly the more I learn, the more I realize I don’t know. It humbles me and I am grateful. Not listening to your patients is the ultimate tragedy in this young gentleman’s story and many stories. He gave them the diagnosis. They did not listen.
Miranda Levy
9 November 2019 • 6:00am
‘I lost a decade of my life to prescription drugs’
https://www.telegraph.co.uk/health-fitness/mind/lost-decade-life-prescription-drugs/
Struggling to come off antidepressants and tranquillisers, and battling withdrawal effects, writer Miranda Levy, 51, thought she was very much alone – until she stumbled on a report officially acknowledging a pill-addiction crisis, and started to find other women with similar stories Prescription-pill addiction is one of the biggest health issues of the day.
This was big news, especially the official acknowledgment of antidepressant withdrawal effects. Suddenly, they came blinking into the sunlight: the ‘middle-class’ prescription addicts who for years had been called attention-seeking by their GPs, with ‘medically unexplained symptoms’. Also vindicated were the sympathetic psychiatrists who’d been seen as outliers with a vendetta against pharmaceutical companies.
‘Oh yes,’ says Healy. ‘Put it this way, if the factories that make these drugs blew up tomorrow, we’d have a serious problem.’
Note to self and others: above is an experienced psychiatric doctor saying that he favours a year of daily intake of diazepam over SSRI.
That says alot to me, in many ways.
And I agree, if used with openness about withdrawal/dependence, benzodiazephines are better to get expected and foreseeable results with, and less likely to produce unwanted results. Caution of overdosing and self-medicating must be applied. Preferably with blood concentration tests each 6 months, if such exists.
And despite benzos has caused many ‘addicts’ and ‘sufferers’ over the years, it also says that we just don’t know how someone will react to a SSRI.
And like Stephen, highlighting how different one person reacts to two drugs in the same family of drugs.
Off topic: my current doctor decietfully grinned at me when I said I had been healthy for 23 years prior to my first visit to psychiatry, -“…but what brought you there?”, he asked….!
Ove2019
Yes Ove, and the said experienced psychiatrist prescribes Diazepam to support a patient when withdrawing from psychiatric drugs, which is extremely helpful. However, the primary care team, who have a written confirmation of this, still refuse to prescribe in such a way that would be supportive. In fact, it’s rather like drawing blood from a stone to get a prescription from them at all – the word Diazepam sends them into a frenzy!
Mary, the spiteful irony for me is that I expressed my own concern when I was first prescribed diazepam, I was terrified to take a pill that I had heard so much bad things about. (And my aunt was, and is, a victim of the 70’s prescription bonanza of them.) So here I was, scared to take a pill that I believed could get me to ‘doze off’ and making me an ‘addict’, and possibly ‘unpersonalize’ me. Meanwhile I eagerly took my 40mg of Seroxat each day, no questions asked, a ‘happy pill’ without a single word of bad rep, and my doctor had only briefly mentioned I couldn’t get addicted to it.
I’m not saying benzo addiction is a laughing matter, but I’d take it over Seroxat addiction any day. And I’ve seen how horribly it affected my aunt, with tremors, stuttered speech,anxiety and inability to sleep and relax.
Coming off Seroxat can give similar problems, but it can also throw you literally ‘off the rails completely’. Not even our expert doctor on this page can explain and describe the complete risks involved. Even though he is closer to the truth than all other so called experts.
We”ll probably never know how many people have suffered the consequences of taking drugs which harmed them, Individuals wouldn’t necessarily make the link unless they are forewarned and medics either poo poo the possibility (look how many at the top of colleges even now do so) or don’t record the truth either too hide errors or ‘they know best’ ie better than what the person is telling them. Many amongst us have only had what we reported decades ago corroborated because others have documented their experiences on blogs such as this. OK the Yellow Card has been useless but there needs to be something where people can report adverse effects independently with confidence they will be recorded accurately . Now notes are computerised and coded they need to be checked to see whether people agree with what has be recorded – or not. Since everything is done to make life simpler for medics there needs to be a check box stating that individuals have given informed consent to taking drugs,( people are entitled to hold copies of notes and in foreward thinking practices can access online)
In desperation, he rang his doctor in his hometown to ask if he should stop the drug —
‘His very words were: “It’s up to you”,’ says Tony.
Tony struggled on until, in July 1997, ‘I suddenly stopped taking the drug and became violently ill.
‘My pulse was racing non-stop. I was terror-struck, suicidal and gripped by a fear that I was going to go completely insane.’
He was admitted to a mental health unit in Hereford, where he stayed for a week. It was a time of ‘utter despair — I just lay there clinging to the bed because I thought that if I didn’t contain myself I might go berserk.’
In the hospital, Tony was given ‘another pill’ — the beginning of an extraordinary journey through many of the drugs familiar to the almost one million people in England identified by the recent PHE report as having been on antidepressants for at least three years — including buspirone, mirtazapine, citalopram and Prozac.
Thousands of patients call on Government to implement 24-hour helpline to tackle the crippling addiction of prescription pills
Niki Jones, Stevie Lewis and Tony Preece each had a dependency on medication
They were left to battle their demons alone for many years without support
Growing pressure on Govt to implement recommendations of a PHE report
By Jonathan Gornall For The Daily Mail
Published: 01:13, 12 November 2019 | Updated: 01:16, 12 November 2019
https://www.dailymail.co.uk/health/article-7674619/Patients-call-Government-implement-helpline-tackle-addiction-prescription-pills.html
Hell was where Stevie Lewis found herself after being prescribed the antidepressant paroxetine at the age of 41 by a GP in December 1996 after she complained of insomnia.
She spent two decades battling to extract herself from the grip of the drug –
Anne-Marie is right in saying that (most – my addition) doctors work hard to help their patients but doctors are on a hiding to nothing.
1. Drug companies want to sell their products and often sale staff are pressured to sell; whether they know or invent claims the doctors hear what the are told. The doctor in this case believed what he tad been taught but there was no comeback against the manafacturer of the improper drug.
2. The human body is extremely complex and we see experts slaving away for years just trying to understand one small facet. Despite many years of training no GP can be expected to understand everything about every possible malfunction of the body let alone know the medication needed.
Two examples: returning from the tropics I spent five days in a hospital which had my records trying to find the cause of pains and failing. .Months later a Norwegian medical student without knowledge of my background saw and immediately realised I had got the same malaria symptoms. Second example: wife of a colleague had a normal birth but never recovered despite every effort of hospital staff. As he was by her side for her last hours a medical student asked if she had been tested for celiac disease; they had not and she recovered
3. During and following the Covid 19 pandemic we hear of and the medical profession pushing “mental problems”. Being ECV I or illness.locked up at home for a year or so but mentally unstable? – no way, Jose**. I see all this public palaver as boosting an invasion of doctors’ surgeries of those who want medicine like those mentioned here “because it is their right” . With doctors’ relative innocence perhaps we are going to see an epidemic worse that the Covid19 problem.
** I think this may be a generational thing. At school during the Cold War some of us were given advanced rescue, fire fighting, radiation and first aid training. Never said, we knew that come the worst it would us to pull the trigger for someone with advanced radiation poisoning. I have had work colleagues badly affected by seeing the results of car crashes – they understood and didn’t need drug “help”. Life now is too sterilized – people just never see or understand death