This post is written by Dr Pedro who is watching events unfold from 10,000 miles away – with some extras added at the end.
The UK Royal College of General Practitioners (RCGP) has been asked by Katy Skerrett, Senior Coroner for Gloucestershire, to respond to her Regulation 28 report to Prevent Future Deaths, after the inquest of Thomas Kingston (above). His death seemed to result from an adverse reaction to the SSRI antidepressants he had been prescribed.
See Aunts, Ants and Regulators, and Who Will Make Medicine Great Again.
It is significant news that the opinion of the RCGP has been thought important enough to be sought. The Royal College motto is Cum Scientia Caritas (Compassion with Science).
Here is a once in a generation chance for the leaders of Primary Care in the UK to improve the lives of patients. Between 15 and 20 % of us in most Western countries are taking antidepressants, mostly of the SSRI type that were implicated in Thomas Kingston’s death.
Action
Dr Richard Vautrey is the current President of the RCGP. He seems to be a reasonable and decent man. His response to the request must contain details of action taken or proposed to be taken, setting out a timetable.
There are two questions to be answered:
- Whether there is adequate communication of the risks of suicide associated with selective serotonin reuptake inhibitor (SSRI) medications.
- Whether the current guidance to persist with SSRI medication or switch to an alternative SSRI is appropriate when no benefit has been achieved and especially when any adverse side effects are being experienced.
Communication of Suicide Risk.
This could be to the doctor or to the patient
Most GPs recognise anaphylactic shock resulting from peanut or penicillin allergy and know what to do. I suspect fewer are aware of the suicidal ideation induced by SSRIs. This I expect is as common as serious penicillin allergy.
We know that printed package inserts, patient information leaflets (PILs) are far too long and most people don’t bother reading them. A dead patient can’t give evidence about what they were told.
The RCGP could announce a plan to provide for training materials or webinars on the subject of “SSRIs and suicide”.
During the initial 4 weeks of treatment should prescriptions be limited to 7 day “starter packs” with review?
SSRI induced suicides are probably more common than valproate induced birth defects. Perhaps reproduce what is now being done to warn of those risks.
Persisting with SSRI Medication
The coroner has an inkling that NICE has got it wrong. Will the RCGP have the guts to agree with her and offer to assist in the urgent rewording of guidance? See the last paragraph below for more on this.
Kingston’s Rule
A few years ago, a child died in hospital from undiagnosed sepsis. Martha had sepsis. Her parents knew she was seriously ill but couldn’t convince the paediatricians caring for her. As a result of her mother’s lobbying, relatives now have a right to demand a second opinion from a specialist when they are concerned that this potentially fatal diagnosis is being overlooked – this is now called Martha’s Rule.
I don’t know but imagine that the number of deaths each year in children from undiagnosed sepsis is less than the number of suicides associated with taking SSRIs.
It’s time for a ”Kingston’s Rule”.
We need a national 24hr SSRI telephone Helpline, staffed by clinicians, specifically aimed at helping people who develop adverse side effects in the first few weeks of taking this type of medication or when their dosage is changed or discontinued.
The PIL would advertise this. Samaritans, MIND, NHS 111 would be required to transfer referrals immediately. People who work for these organisations would be trained in recognising akathisia and its management.
Handing out a similar leaflet to the ones that must now be given to women taking valproate could be mandatory. This could give akathisia information and advice as to when to call the helpline.
It seems that the RCGP is not in the business of issuing advice at the moment and defers to MHRA, NICE and RCPsych – Mental Health Toolkit.
The RCGP must grasp the nettle and help minimise suicides triggered by adverse reactions to SSRIs.
Putting the clock back
Depression was a rare disease in general practice, when I began there. Instead people complained that they couldn’t sleep. Probably the last time GPs got their act together was in the mid-70s when they proposed a successful voluntary ban on barbiturates – sedatives that commonly led to fatalities in overdose.
The barbiturate gap was filled with -azepams etc. Valium, Librium, Mandrax, Doriden, Dalmane are just some names that come to mind. (These were for the younger patients, the older ones could be fobbed off with “tonics” perhaps with vitamins and iron.)
The tolerance and addictive properties of these drugs were soon realised, GP records were, and still are full of stern warnings – “Diazepam 5mg x7 NOT to be repeated – which they inevitably are by a different doctor.
Then word got out that these patients were depressed and needed a short course of antidepressants and the -azepams must be stopped. First a month’s treatment was needed. Then we were told 6-12 months was better to prevent relapse. Tricyclics were best. Amitriptyline gave a dry mouth, so patients knew they were on a real drug. We learnt never to refer a patient to a psychiatrist until they had tried that doctor’s personal favourite. So I issued prescriptions for a fair bit of clomipramine – Anafranil.
Although we never used them it was about this time that various depression rating scales came in. These were invented by pharma as research tools. True family doctors needed no such thing to determine whether their patient was depressed.
Then scientists discovered that depression was due to brain serotonin levels being abnormal. The great news was this could be corrected by SSRIs and make patients great again.
In the early part of my career we could refer patients to Community Psychiatric Nurses. They indulged in talking therapies – although that term was not used in those days. These poorly paid sensible people had minimal training and used common sense and sympathy to help people. This was before counselling and CBT came on the menu.
My impression, throughout my career, was that from the effectiveness point of view – all the treatments – tablets or talking were about as good or useless as the others.
We know that one of the best antidepressant treatments is placebo. At least 80% as good as any drug it has been compared with, and a safety profile to die for. In the 1960s GPs could prescribe aspirin flavum – yellow aspirin – when they didn’t know how to help someone, and I remember a trial which showed that red placebos were better than other coloured analgesics.
What did I learn?
- Most people got better
- Depression often affected a family – you only had to treat one person in the family and all would improve. Relatives were relieved that something was being done
- “Depression” can be the first sign of Parkinson disease or cancer
- Young people with learning difficulties often appear depressed but aren’t.
- I have no idea what compliance was like
- Male impotence was occasionally discussed “temporary” and PSSD did not exist.
- I still don’t understand how antidepressants help depressed people with cancer regardless of their serotonin levels. Give me a glass of wine, preferably ice-cold with bubbles.
- If consulting a certain patient makes you feel depressed s/he probably has social problems
There was a recent article in the British J of General Practice – What are the Challenges to Quality in modern hybrid General Practice?
The (young) editor of the journal, Euan Lawson, clearly thought it was great and that it should have what is apparently a new buzz word linked to it – Enshittification – see this link for where this word came from and what the editor sees in the article.
The article is jargon-overloaded but states what we all know – that general practice is extinct and what’s on offer is not fit for purpose. Sadly, todays GPs don’t realise what they’re missing by not getting to know their patients.
It reminds me of a tour I did in 1972 of the Soviet Union where the Intourist guide told us that men became Orthodox priests because the job paid well, implying they had no religious faith..
How would I advise Dr Vautrey?
I wouldn’t be surprised if he didn’t recognise the word akathisia. I wouldn’t have until recently. I would still not be sure how to treat SSRI induced suicidality – akathisia.
He might like to survey the membership and patient organisations to gather evidence of the SSRI problems and gather suggestions to prevent future deaths. It would be good if there was a “family members– bereaved by suicide group” he could contact, although the risk is that these all now promote the use of antidepressants.
Readers of this blog could send him suggestions. His email is in the public domain.
The RCPsych has led the way in its rearguard action to delay acknowledging SSRI problems and has done little to minimise overdiagnosis and overtreatment of “low mood”. Does Dr Vautrey feel strong enough to stand up to his opposite number in RCPsych? Almost all new antidepressant prescriptions are initiated in primary care.
Assuming that he knows that virtually all the literature about SSRIs is ghostwritten by industry employees – would it help to explain this to the coroner?
Could he ask the Coroner to persuade Government to legislate so that raw data from clinical trials is made freely available?
Could he suggest to the Coroner that whatever NICE says, the advice they give is unhelpful.
In particular – in the case of a depressed young person who already feels suicidal and is prescribed an SSRI – a warning that during the first few days your symptoms may get worse can at present only lead to a doubling of the dose.
Could he suggest that organisations like NHS111 and Samaritans are made aware and receive training about SSRI suicide risk?
One of the tricky bits is the question about wandering into territory when the lawyers say don’t say it looks like the drug caused the death.
Coroners need to insist that the GP who issued the prescription gives evidence in court. Doctors will of course develop PTSD or depression, maybe even dementia.
Still – the question needs to be asked. Do you think it is possible that the SSRI triggered suicidal thoughts?
The Coda here was not written by Dr Pedro. Apologies for the change in tone.
CODA

It usually takes parents or families to create a Martha’s Rule but in this case the central people may be Katy Skerrett or Richard Vautrey. Ms. Skerrett’s report joins over 40 Other Coroners concerned about the drugs Tom Kingston was on.
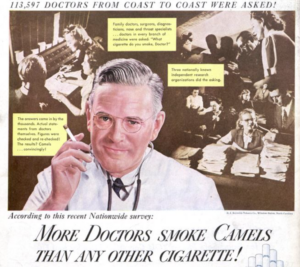
What Ms. Skerrett and Dr. Vautrey are up against is caught in the famous image below.
That was 1962. Today the BMJ, the journal of the British medical profession, whose pages are festooned with adverts selling a Camel Veoza getting through the eye of a needle, are scared to even hint at the fact that treatments may have harms. So much so that they can run an ‘educational’ article on Assessment and Management of Self-Harm in Young People by Mughal et al that mentions nothing about keeping an eye out for adverse responses to SSRIs and how to manage them.
I heard about this article which appeared between Thomas Kingston’s death and his inquest, because the parents of some teenagers, who had been put on SSRIs and died, drew it to my attention. I’ve just read it today.
Marion Brown, Tim Moss and Vincent Schmitt submitted some truly Great Responses to the article which can be seen in full in the GR link. BMJ were very slow to publish any of them. Then bizarrely a week ahead of Tom Kingston’s inquest, BMJ sniffily added its own extraordinary response and have resolutely refused any follow up responses:
Adverse effects of medication were not the focus of this education article. It was based on the new NICE guidance for self-harm, which was primarily focused on psychosocial factors and care rather than pharmacological treatment.
BMJ Editors. Competing interests: No competing interests
BMJ editors who avoid putting their names in the frame have the gall to write no competing interests when its almost impossible to read BMJ these days without being interrupted by pop up and other adverts or educational sessions for Veoza, rapid responses to which they have also been refusing to publish, and for Lilly’s Kisunla – see Hope, Hype, Consent and Alzheimer’s.
Worse again BMJ recently featured an in the circumstances deeply hypocritical editorial on Predatory Journals: what can we do to protect their prey? Their Prey? It is difficult to avoid the impression that this is all about money – BMJ and the other journal editors who wrote this want the money that goes with Open Access publication.
Open Access does not mean you get to see the company data behind a publication as the norms of science suggest you should be able to – it means you or your institution hand over thousands of dollars so others can download this article for free and get told they really must get put on this drug which can only benefit and is close to completely free of adverse effects. Of course pharma have more money to hand over than anyone else in order to get messages like this out branded as ‘science’.
The appalling predatory journals, BMJ etc complain about, have arisen because some smart folk have looked at BMJ and NEJM’s no-brainer business model. The predators Prey? They at least will publish anything for money – even the adverse effects of treatment. They may be keeping some people safer than BMJ/NEJM etc.
BMJ and NEJM and other major journals should be designated as Zombie Journals – perhaps both Zombie and Predatory. It may be time to face the fact that we don’t really have any decent medical journals these days – we have businesses that have a journal front but we do not have journals – see Silencing Doctors, Silencing Safety.
The result is Clare Gerada a former president of RCGP and Tony Blair (giving medical advice) have just featured in a Daily Mail article about Britain drowning in a tsunami of labels and psychotropic meds. C and T are blaming patients for seeking out meds and labels. Portraying medicines as sacraments – something that can only do good and cannot harm – cannot result in anything other than this outcome. But neither Clare nor Tony mention this.
Luther Terry, the Surgeon General in America, the kind of doctor we had before1991 when Richard Smith and BMJ told doctors their views were anecdotal, helped turn the tide on a comparable problem in 1964 by openly stating in a way that could not be ignored that Smoking can Kill.
Dr Pedro sees SSRI induced deaths as relatively rare. I think deaths from these and related drugs rival smoking induced deaths from lung cancer and heart attacks combined in frequency.
Two more BJGP snippets. One was close to a repeat BMJ Mughal et al article, also by Mughal et al – How GPs can help young people avoid future self-harm. This interviewed 15 family doctors none of whom seem to have heard about possible adverse responses to antidepressants. This came out nearly 5 months after the BMJ article by the same authors and the responses from Marion, Tim and Vincent pointing to its problems. There is not a hint that anything has penetrated through.
A second snippet in BJGP this week covered Antidepressant Follow Up a point that concerned Katy Skerrett. Its author mentions a survey of 17000 people starting an antidepressant which reported that:
- 28% of patients were followed up within 14 days,
- 51% within 30 days,
- 67% within 90 days of first drug dispensing.
The other 33%? At least 33% will have had the wit, as Tom Kingston had, to stop a treatment that was not suiting them and fortunately, unlike him, will have opted not to report back to their doctor. Among the 67%, some will have had the sense to lie to their doctors – even doctors like the 15 Mughal et al interviewed who rather smugly seem to think they do a pretty good job.



Thanks Dr Pedro! I find your paper very relevant. I am one of the authors of the rapid responses to the BMJ paper you mentioned above.
There is a little story about my RR.
The **peer-review** according to BMJ.
My wife Yoko wrote first a RR to BMJ, I think she explained our son’s case Romain. (He died by suicide induced by paroxetine.) She also explained directly that she knew at least 20 other suicide or suicidal cases due to SSRI, or something like that.
Her RR was rejected with the arguments that the victims were not **peer-reviewed**.
Then I tried myself to submit my RR to BMJ, using another approach: pompously calling myself a mathematician — authority argument !! — and arguing about the scientific content of the paper. Nothing got published right after my online submission… So I resent my RR in a common email to all authors and to the editor. Then once, it got published.
One month later we got this unique answer from BMJ that everything stands in this paper because it is **peer-reviewed**. Even if the paper is evidently problematic.
In brief the **peer-review** label is used to support fake arguments.
Once statements are peer-reviewed, they become truth, words of gospel.
This is really a problem.
Thank you for this hugely important blog post
Could I just add a link to my e-letter response that BJGP published at end December 2024.
https://bjgp.org/content/74/749/e832/tab-e-letters#no-effective-interventions-to-reduce-repeat-self-harm-behaviour
As yet there seem to have been no other e-letters relating to the BJGP Mughal et al article – which is highly alarming in revealing the GP views featured.
From Annie Bevan
Great Reporting, Dr. Pedro. I have always been pleased to see you in our Comments section.
All these years the cover-up of harms and deaths from antidepressants: Royal College of GPs, Royal College of Psychiatrists, NICE, MHRA, Medical Journals, et al.
Simon Wessely, Clare Gerada, Louis Appleby. The famous voices with the accolades.
This, it must be said, had a powerful influence over the media reporting. And would have influenced the NICE people, who don’t have a clue.
Thomas Kingston’s death has sparked a massive media frenzy, being of noble bearing. It really shouldn’t have taken this man’s death to light the spark.
Kingston’s Rule is a great idea.
There seems to be this huge juggernaut of denial to change and you have come up with some good ideas. Coroners have a limit to their powers as been written about.
From personal experience, I know how loose and sloppy doctors can be, even when it’s obvious.
I think it’s got to the point that Doctors will have to be Dictated to. Told, instructed, and warned if they don’t pay attention to all the points laid out.
And that means changing and challenging everything that has been lapse and ignored for so long.
I thought Marion, Tim and Vincent’s replies were extremely robust.
This whole saga needs a breath of fresh air from all organizations, who are so reluctant to take a real lead. Let’s hope there are some courageous people with leadership capabilities who will take it on.
I was founder (trainee) member of the JCPTGP – Joint Committee on Post Graduate Training for General Practice (1975 – 1978).
We moved the (GP) Vocational Training Bill from Green Paper to Statute.
The RCGP team were formidable in their commitment to improve training and standards in General Practice with a three year post graduate rotation through outstanding Training Practices – twelve months, and a two year rotation through four, highly relevant hospital specialities)
Educational achievement was assessed by examination for the MRCGP qualification.
For many, this sophisticated training opportunity became a first choice career pathway. often for top graduates.
Elite Vocational Training Scheme places became highly competitive.
The JCPTGP survived for 40 years. I regret that this renaissance in General Practice – Cum Scientia Caritas – appears to have been followed by ‘Guideline Dictated Practice’, presumed to be ‘Evidence Based’ Practice.
I believe that the JCPTGP would have taken our concerns on board, and ensured that trainees were aware of these ADRs, and how to avoid and/or manage them.
Tim
Can you see any way forward for RCGP now? The awareness among family doctors that psychotropic drugs have side effects, never might potentially lethal ones seems all but non-existent. Either that or our freedom to talk about these things has disappeared completely. How do we break out of this death spiral?
David
This is a challenging question.
There has surely got to be a tipping point where so many have been killed, or their lives have been destroyed (including doctors themselves), where
AKATHISIA DENIAL is no longer tolerated by patients and their families.
It feels as if there may be a snowball effect now developing, increased by the Coroner’s publicised Prevention of Future Deaths Report re Tom Kingston’s death.
Medical journalists may find an opportunity to address a forbidden subject. Journalists covering the Royal Family may ‘add snow’?
I have often, sadly, felt that litigation is a powerful driver of change in medical practice.
Litigation for antidepressant induced suffering and death seems to be beyond our reach.
Eventually perhaps legal firms bringing class action may be looking for those of us who comment here?
Your life’s work has given us a real Evidence Base. We have to ‘keep on keeping on’ like a dripping tap.
I felt that the MISSD London Underground Akathisia advertisements were brilliant.
When all the laity know this term, we can all inform prescribers.
Re the RCGP, there has previously been very powerful, high office advocacy in favour of SSRIs/ADs.
An editorial in BJGP written by Professor David Healy could be invaluable, and we need to find ways of educating Vocational Trainees in General Practice that ADRs to these drugs are a preventable, avoidable and (at worst) a manageable cause of akathisia, disinhibition, emotional blunting and iatrogenic death and maiming.
I have come to believe that no trainee should be accredited in General Practice without detailed knowledge and awareness of prescription drug induced self harm and violence to self or others. It should be mandatory VTS teaching and learning.
That is: We need to prevent the SSRI prescribing habit (an invaluable means of getting a patient out of the consulting room) before it becomes established.
Tim As somebody with knowledge of how it is decided what goes into the training of doctors – It seemed that you were able to set something up Would it be likely that a CPD module would find any support.? How or who would it need to be proposed by. Maybe enough doctors themselves would welcome this?
Freedom to talk about these things:
is like watching One Flew Over The Cuckoo’s Nest and expecting a different plot line and ending.
Freedom to talk, freedom to take evidence to consultations, is possible as is the freedom of refusal to provide a service, or the freedom of power to label, diagnose, institutionalise ….
There are freedoms but they are selective as to who can access them and for how long and for what purpose and for whose benefit and gain
The JCPTGP: the passing of an era Brian Keighley Br J Gen Pract. 2005 Dec 1;55(521):970–971.
https://bjgp.org/content/55/521/970
On 30 September 2005 the medical regulatory body with a famously forgettable acronym, the Joint Committee on Postgraduate Training for General Practice, was gently and sadly laid to rest.
GP educators universally referred to this UK-wide organisation, which for a generation held pole position in quality assurance of general practice, as the ‘Joint Committee’. It was, however, never accorded its alphabetic or historical seniority when bracketed with its sister organisation, the Specialist Training Authority (STA); both being competent authorities for assuring medical training under the European medical directives (specialist training under Article 3, and general practice under Article 4).
The JCPTGP was a unique body that brought together not only the then divided tribes of general practice (it was a joint committee between the Royal College of General Practitioners [RCGP] and the General Practitioners Committee [GPC]), but also had representation from GP education directors, postgraduate deans, specialists, doctors in training, the Departments of Health and, latterly, the laity.
The leadership of the JCPTGP alternated between chairmen appointed by its two parents, the RCGP and GPC, and had two medical joint honorary secretaries, one from each. Its signal achievement was to unite disparate medical organisations under a single banner of excellence within general practice and it was always known for the quality of its quarterly debates.
Unlike the STA, the Joint Committee had to survive on a grant-in-aid from the Department of Health (often remitted late and well into the financial year) together with a donation from the RCGP to support its standard-setting function.
The Joint Committee, in contrast to many specialist medical royal colleges developed a respected methodology for quality assurance that was economic with the resources of the organisations it inspected. Rather than examining every individual medical post, the JCPTGP inspected deaneries and their systems for ensuring quality GP training, and only sampled the posts within them. This was held up as an exemplar by many, including successive Chief Medical Officers (England) and contributed to limiting the ‘inspectionitis’ that many within the NHS feel reduces time for patient care.
Over its 30 years of existence the Joint Committee achieved two other major breakthroughs.
The first was the refinement of its regulatory powers with the introduction of new Vocational Training Regulations in 1998…
The second major breakthrough was the introduction of summative assessment of training, under the same amendments to the regulations, in the teeth of opposition from elements within the GPC. Until that date, a doctor’s general practice training was entirely experiential — if the doctor had undertaken certain prescribed medical jobs, he or she gained a certificate by default, without any test of competence. Summative assessment tested consulting skills usually by watching a video recording of the doctor at work with real patients, technical skills, and examined written evidence (usually by conducting a clinical audit). It also tested the ability to apply new knowledge learnt over time as assessed by the trainer…
We now face a new era with Modernising Medical Careers and a new unified regulator, the PMETB… If they fail, they will have been profligate with the proud tradition of excellence and endeavour they have inherited from a JCPTGP that represented the very best features of cooperative working and mutual respect among doctors and lay members who worked tirelessly towards public protection and best training.
Thank you for this comment Steve.
As I read it, I recollected the voices and faces of some of the ‘Joint Committee’s inspirational GPs who fired my enthusiasm as a recently appointed Vocational Trainee in Northumberland.
I found that G.P. vocational training provided a brilliant preparation for a return to hospital practice, and this, plus the work we completed in the JCPTGP on defining the ideal educational content of a hospital GP Training post lead me to establish such a post, and to be inspired by our VTS trainee’s sophisticated consultation skills, and their developing clinical skills, for many years.
Re Anon comment above:
I am certain that our trainees would have been receptive to a CPD module addressing akathisia and its sequelae. They could have then adjusted their prescribing in a safer direction throughout their Primary Care careers.
I knew nothing about these ADRs at that time. There was no RxISK to learn from in those days.
It would appear that the problem is not with the learners, but with a rigid defence of antidepressant drugs at the highest college level.
I find this ‘academic certitude’ incompatible with the philosophy of the JCPT in the 1970’s.
Thank you for correcting me. The Joint Committee survived for 30, not for 40 years.
Thank you Tim Would it be possible for a group of retired or non practicing doctors and others with the know to put a module together unofficially ,which could then be accessed informally without the need for approval from colleges and so on. Something with a structure.
This is not Tim responding – there are a few problems with this idea. First even when practising family doctors don’t get to meet in groups where they can share concerns and put something together. Second, after retiring this is doubly so – plus they are not seeing the things you’re suggesting they put something together about unless it affects a family member in which case they are conflicted. Third they dont have a distribution channel – without a distribution channel nothing anyone puts together does anywhere
D
I interviewed Dr. Kirsch for my second book and I wholeheartedly agree with his assessment: doctors should write no new prescriptions for antidepressants. As for the patients who are already taking them and say they are doing well, leave ’em alone (especially since most doctors know so little about getting people off these drugs safely). But doctors should do no new prescribing. The short-term benefits of AD’s, as demonstrated in randomized controlled trials bought and paid for by the drugmakers, can be replicated in full by any of a variety of nondrug means, without any of the toxic effects. In the long term, these drugs cause worsening depression and in a few patients, cause a state of agitation that can lead to suicide and homicide.
I applaud you, Dr Pedro, wherever you are – 10,000 miles away. You have come up with the sort of BIG communications’ idea that’s needed to cut through the confusion, contradictions and dangerous nonsense that beset SRRI ‘safety and efficacy’ messaging to doctors as much as patients.
I’ve found this extremely revealing NICE qualitative (28 studies) evidence review (2022) of PATIENTS’ PERCEPTIONS of the information and support delivered to them by HCPs when prescribing antidepressants. What information? What support? It’s a shocker:
‘Although some described antidepressants as being a natural and bodily substance that could do no harm, the vast majority of people appeared worried about the dangers of being on antidepressants long-term and questioned why they had not been told. Several reflected on how they had not been warned about side-effects, how GPs had neglected to inform them when the medication was prescribed and how this lack of communication was a source of worry.’
‘Some had fears of becoming addicted to medication or that it would seriously reduce their alertness or change their personality. Many reported various side effects which they considered most troubling to them such as dizziness and sleep disruption, others highlighted they had lost their thinking capability,and/or memory as a result of long-term antidepressant medicines or experienced unexpected difficulties in performing their routine work while they were taking medicines. Adverse effects often appeared to amplify the degree of dissatisfaction with doctors or the health care system or altered their medicine behaviour (e.g.leading to discontinuation or withdrawal).
WOMEN STRUGGLING WITH SEXUAL DIFFICULTIES at an early stage of medication in particular, who had not been informed about them by their GPs, questioned whether their experiences were normal and felt that having more information at an early stage would have assisted them in coping’.
https://www.nice.org.uk/guidance/ng215/evidence/a-patient-information-and-support-pdf-11018568638
David observes, ‘The awareness among family doctors that psychotropic drugs have side effects, never mind potentially lethal ones seems all but non-existent. Either that or our freedom to talk about these things has disappeared completely..’ Quite honestly, my impression is it’s the former. For all sorts of reasons, not least of all that pharmacomythology is presumably baked into this generation’s medical education, the guidance is overwhelmingly ambiguous, ideological wars re withdrawal etc. rage and probably cancel each other out in the overburdened autopilot GP consciousness, seeing on average 37 patients a day : https://www.pulsetoday.co.uk/news/workload/40-of-gp-practices-set-limit-on-number-of-patients-seen-per-day/
So back to the cut through clarity of Dr Pedro’s BIG idea. There can’t be many people in this country who don’t have the image of Tom Kingston imprinted on their minds and his ghastly SSRI induced fate. The image is articulate – his doctor had no idea of the risks and he wasn’t informed – this could happen to you or someone you love dearly.
It could elevate safety communications to a whole different level If the family felt able to get behind an idea like “Kingston’s or Tom Kingston’s Rule’ – after all ,it’s no different from Lady Gabriella’s press statement – ‘I believe anyone taking pills such as these need to be made more aware of the side effects to prevent any future deaths. If this could happen to Tom this could happen to anyone.’
In the event it’s a bridge too far for the Windsors, perhaps Dr Pedro could create another BIG idea – I don’t have the talent – and can only think of something prosaic along the lines of the Antidepressant – Start, Stop, Switch Rule.
It’s a perfect moment with the MHRA rising to the political challenge of reviewing antidepressant safety comms. They are making it their business to consult bereaved families and suicide prevention groups .It would be great to see extremely experienced and knowledgeable campaigners like Marion and Tim having an input., as well as recently bereaved families like Yoko and Vincent.
I also liked Dr Pedro’s idea of limiting initial prescriptions to 7 days ‘ worth– but wonder if a daily pick up from the pharmacy for the first 28 days night be safer, although logistically a bit tedious. Pharmacists are stepping into the medical breach a lot more as we know – and ,unsurprisingly, given their profession, they seem better educated in pharmaceutical effects than many doctors.
Ofc the other big point we keep touching on is – even IF SSRI induced suicide/suicidality did only affect a minority of patients – we can never know this accurately, since it is so consistently misdiagnosed as the balance of the patient’s mind being disturbed (actually rather accurate at a psychopharmacological level) – all patients are exposed to this same risk because we can’t individualise it.
What we can do is produce simple lucid guidance telling prescribers and patients – if your patient/you feel like this – overwhelmingly turmoiled and agitated, suicidal at the same time as emotionally indifferent, intensely manic etc., get help urgently, don’t let anyone increase the dose or switch you to a drug in the same class.
Dr. Pedro (a/k/a retired NHS GP Peter Selley) wrote an open letter to the Royal Colleges of GPs, outlining his call to action on SSRI’s and suicide.
It just got published in the BMJ, in the form of a Rapid Response to their news article on the coroner’s report in the death of Tom Kingston. Along with a letter from David Healy on the worrisome rise in SSRI’s prescribed to youth in Australia — young women especially.
https://www.bmj.com/content/388/bmj.r67/rapid-responses
Looks like the word may be getting out! Hope it will increase the pressure on the RCGP to take action. They can be contacted on Twitter/X as follows:
@RCGP @BJGPJournal @rvautrey @KamilaRCGP (and @ClareGerada for good measure)
At first, I misread this, thinking that Harriet was highlighting ‘rage’ itself as possibly part of the adverse effects seen with some drugs used to treat depression or anxiety. It seems to me that this rage, whether directed inwards to self by suicide, or outwards in acts of violence towards others, has to be understood before there is a will to prevent it.
I agree that family doctors, however overworked, definitely need to develop a complete understanding of these drugs. Individuals need to understand that which they choose to prescribe.
However, a groundswell of knowledgeable public pressure is also required, if there is going to be social change. Such change could include the future increased likelihood of successful legal actions possibly in the delict of negligence.
Akathisia: This needs to be described more fully, if the general public is to grasp the full meaning of this, and how it relates to the other adverse effects, and how it is of concern to them as individuals in terms of safety.
Disinhibition: What exactly is meant by the ‘disinhibition’ sometimes caused by certain prescription drugs? I think that the range of disinhibited behaviours needs to be spelled out more clearly. Is this sometimes manifested as verbal inappropriateness, sometimes by physical violence?
Emotional blunting: How might this be described, and how may a person spot this in a loved one’s demeanour?
Tim proceeds to say: ‘I have come to believe that no trainee should be accredited in General Practice without detailed knowledge and awareness of prescription drug induced self harm and violence to self or others. It should be mandatory VTS teaching and learning.’
It is also a tragedy that Tom Kingston died in a violent suicide.
Dr Pedro writes an informative post, with a good suggestion that a Kingston’s Rule be implemented, in an attempt to stop SSRI induced deaths.
Dr Pedro writes: ‘How would I advise Dr Vautrey?
I wouldn’t be surprised if he didn’t recognise the word akathisia. I wouldn’t have until recently. I would still not be sure how to treat SSRI induced suicidality – akathisia.’
This, I think, is one crux of the problem. Even if 24 hour helplines were indeed reliably set up, what would be the possible ranges of urgent treatment for this psychiatric emergency?
It’s not the crux of the problem. The crux of the problem is family doctors see people get worse and have been threatened into not recognizing this as an adverse effect of treatment – no amount of education is going to change this while BMJ, BJGP etc on the advice of their lawyers strenuously avoid linking medicines to hazards. A lot of this is covered on RxISK – there are tons of posts about akathisia and disinhibition. Wendy Dolin and MISSD have put adverts on London buses about akathisia. Repetitive orgasms normally sell – except when linked to meds. What blocks so many from registering the message?
D
In most of the coverage of the Kingston case at the bottom there is a link to Samaritans. There needs to be a link to here and rxisk. The information that we post will help people.
Re: understanding what akathisia is when even the sufferers don’t grasp it. For starters I would use Antonioni’s Zabriskie Point:
https://m.youtube.com/watch?v=guOmJM8xvHA
With the words: This is what Akathisia looks like inside a person’s head that you can’t see or hear.
Chris
The link to the Samaritans or other suicide helplines etc as things stand is dangerous and likely kills people
David
https://opmed.doximity.com/articles/it-had-me-by-the-hair-and-wouldn-t-let-go-parsing-an-unusual-suicide-phenotype
The above article, along with similar ones, is written by an American psychiatrist.
Acute Adjustment Disorder (Young People) Akathisia Suicide Attempt.
He makes mention of akathisia, explores the various aetiologies, and likens the phenomenon explored here to the akathisia linked to the use of SSRIs.
He describes the restlessness, extrapyramidal motor overactivity, lack of previously expressed suicidal ideation, and no memory of the act itself after being successfully resuscitated in hospital.
The young patient of the title later reported ‘it had me by the hair, wouldn’t let me go, I was being dragged to my doom’.
The point that I am making is that this author effortlessly compares and contrasts the different causative agents of akathisia, casually mentioning the SSRI antidepressants being linked to akathisia.
This he does in order to make the rare phenomenon (and to suggest similar pharmaceutical treatment for) of purely psychologically induced, ie adjustment disorder, suicidal akathisia clearer.
This psychiatrist’s research is interesting, and is not all perhaps as recent as we might prefer.
I think that the message has existed among the profession for quite some time, perhaps subliminally.
The way things are going it’s more like a death spiral of medicine, as you said before, so more Thanatos than Eros.
The only answer is to build on the momentum of poor Tom Kingston’s tragedy.
To Dr David Healy, Dr. Pedro, Vincent and et al.,
Unless the tail is amputated it will keep on wagging and even when amputated the stump will keep on wiggling. And so to keep chasing after what has already been is exhausting surely?
A shift of larger degrees is needed; not a repeatedly reformulated hypothesis, theory, with gaps being filled with like-minded matter.
Children need their parent, parents, full stop.
Children lose their way because everything, everything, about child care is farmed out to others. Parents have fallen for this zeitgeist.
There is no, not one, contributing factor to life – and yet each new article, opinion, therapy professed by “experts” regardless of who they are or their lack of transparency, is pounced on as if it were the missing link.
Life in its simplest form and in its most complex form requires immediate attention at all times, but especially so in trickier moments. This ask is beyond a child’s capability and capacity. Parent substitutes such as teachers, educators, (and doctors) have a lot to answer for; starting often from 6 weeks of age.
Maybe in a few more decades or even hundred or so years, the biology of warmth, nurturance, healthy attunement, affection can be smothered out of the cells of humans, thus proving “science” right.
When an infant, child, adolescent is in distress they need instant support.
The quick fix is school interventions, psychology assessments, and drugs.
Stop handing over the child’s life to orhers!
Just one example – When schools offer funding for services to help with a child’s “problems”, they are serving themselves with the money they receive. If asked for evidence on what is provided, nothing can be shown that is of short or long term value.
Trapped by mandates of compulsory attendance for education plus commitments of work, family, income, bills, debts, holidays, not missing out ….. [We] hand over care to those whose best interests do not serve the child (or their family).
Doctors work for profits. They work to strict time key performance indexes. Their every minute, every key stroke, every decision is monitored, assessed, evaluted, recorded – who can work like that and with governed, mandated, …., restricted options?
Private practices run differently depending on whether they are fully private or receive some financial benefits.
When noticing something unusual about a child, it is difficult to prioritise them when other’s have their own solutions that primarily serve them and their sway is dominant. Often options and choices are minimised creating a narrow lens of either this or that.
The fear factor is well entrenched that if something is not done immediately, pressure pressure pressure, then something bad or terrible will happen. And if something bad or terrible happens it will be the parents who are at fault and to blame.
Prescibers are never held to account – they are well protected. They have a multitude of ways out of their “unintended” harms.
Laws take these Regulations into account, and policies also oblige.
Sad, sad, – and criminal.
People of affluence are brought to light because they are in a position to sue. News-worthy. A possible blight on a Nations national and international report card.
The everyday common public are just that – the everyday common public.
All those service centres and referral centres that are being set up by their hundreds are doing what? – Housing a few employees; allowing providers to claim rent and other deductions, …
So the real reality is that health is wealth-bound, power and control bound, and is kept at an optimum by ideology.
What dose a mother do?!! One adult son with A major break down. – – you name it. We have it ! one other with severe L. d. Where do we go from here. ? ( I know you are right)
From Marion’s X/twitter
Rapid response to:
Coroner questions advice on risk of suicide with SSRIs after death of financier
BMJ 2025; 388 doi: https://doi.org/10.1136/bmj.r67 (Published 13 January 2025)Cite this as: BMJ 2025;388:r67
19 January 2025
David Healy
https://www.bmj.com/content/388/bmj.r67/rr
Dear Editor
Recent data from Australia show that over the last decade there has been a switch in profile of new users put on antidepressants. The incidence rates for new use in those aged from 45 up to 85+ were over double the rates for those under 45. Between 2015 and 2023, this has changed; the incidence rate for those under 45 is now higher than for those over this age – Thomas Kingston’s age at the time of his death (1, 2). – among whom there has been a fall in new use.
The good news is that this change likely stems in part from efforts to avoid polypharmacy in older people. The rise in incidence among younger people – a 100% rise among the youngest women – for whom the evidence that these drugs help is less convincing. is more problematic.
A recent paper looking at the knowledge of and comfort levels of family doctors when dealing with self-harm shows no awareness of the issues that concerned the coroner in the Kingston case (3). Engaging with the coroner’s call will be a challenge for RCGP. Emerging data, however, suggest that skill in handling the adverse effects of antidepressants is increasingly needed.
1. Costa J et al. Changes in antidepressant use in Australia: A nationwide analysis (2015-2021). Aus & N.Z. J. Psychiatry 2023; 57; 49-57.
2. Costa J et al. Antidepressant use among Australians between 2015 and 2023: An updated analysis. Available from Juliana de Oliveira Costa j.costa@unsw.edu.au
3. Mughal F et al. How GPs can help young people avoid future self-harm/ Brit J Gen Practice 2024, e834.
Competing interests: No competing interests
If this is the prevailing narrative in the press, then there is a long way to go
The Telegraph
What you should know before starting antidepressants
How often do you take them, what are the side effects and when could you start to feel better?
https://www.telegraph.co.uk/health-fitness/wellbeing/mental-health/everything-to-know-about-antidepressants/?msockid=29600be03a226e1b15531ed83b056f25
https://archive.is/XsrR0
“Antidepressant is an umbrella term that includes several classes of drugs, but there are similarities in how they work,” says Carmine Pariante, professor of biological psychiatry and a spokesperson for the Royal College of Psychiatrists.
“All antidepressants work by changing the function of chemicals that brain cells use to communicate,” Prof Pariante explains. As a result, antidepressants reduce the hyper-activation of areas in the brain that are associated with sadness or anxiety and help to reduce negative thinking.
Selective serotonin reuptake inhibitors are believed to work by increasing the level of serotonin (a mood stabiliser) in the brain. Serotonin is usually ‘reabsorbed’ by nerve cells after carrying a message between them – these block that reuptake.
Examples: citalopram, fluoxetine (brand name Prozac), sertraline
If you find that the side effects aren’t settling down, Krishan says, contact your GP. It may be that one particular antidepressant, or class of antidepressants, doesn’t agree with you. Your doctor will be able to recommend an alternative.
If you feel there hasn’t been a significant improvement after a few weeks on your initial dose, your GP may suggest increasing it.
By KATINKA BLACKFORD NEWMAN FOR THE DAILY MAIL
Published: 01:30, 21 January 2025 | Updated: 01:30, 21 January 2025
A facial at a beauty clinic left me suicidal, then I was arrested and finally sectioned – all because I was given antidepressants that I didn’t even need…
https://www.dailymail.co.uk/health/article-14305699/facial-clinic-left-suicidal-antidepressants.html
The night she took her first dose she woke an hour later ‘feeling like I couldn’t breathe. It was as if my airways were closing. My body was burning from the inside out, and I had this terrifying sense of being under attack,’ says Laura.
What she is describing is akathisia, a rare but severe reaction to medication (including, but not limited to, antidepressants) that causes constant agitation, an inability to stay still, and a consuming sense of terror.
‘It was like swallowing hell in a bottle,’ she says. ‘I felt like I was being tortured from the inside. I couldn’t sleep, and I was pacing around like a caged animal.’
Dr Simon Opher, MP for Stroud and chairman of the Beyond Pills All Party Parliamentary Group, told Good Health: ‘Suicide has always been a known side-effect of antidepressants. The tragic case of Thomas Kingston has highlighted the need for the dangers of these drugs to be made more overt, with warnings on the packaging and with better education for both doctors and patients.’
For years, Good Health has been highlighting the alarming link between suicidal thoughts and SSRIs (selective serotonin reuptake inhibitors), the class of antidepressants that include sertraline and citalopram.
A few weeks after the neurologist had changed her prescription, Laura saw her GP, who diagnosed anxiety and depression, and prescribed additional medications, including the anticonvulsant pregabalin and another antidepressant, mirtazapine, a type of drug known as a tetracyclic. ‘This pushed me over the edge,’ she recalls. ‘The terror became unbearable. I was researching suicide online, convinced there was no way out.’
I hear from people like Laura every week through antidepressantrisks.org, the non-profit website I set up with experts after I suffered a catastrophic reaction to an SSRI.
Tragically, as in Laura’s case and my own, their medication-induced reactions are often misdiagnosed as mental illness.
‘Nobody listened when I said it was the medication causing my symptoms,’ says Laura. ‘If
they had, I could have been spared so much suffering. These drugs can make people want to kill themselves and people need to know this.’
Deadly side effects being ‘hidden’ from patients by drug firms –
https://www.dailymail.co.uk/health/article-14308007/Deadly-effects-hidden-patients-drug-firms-Ozempic.html
The MHRA and the whole of the health industry are swimming in a sea of pharmaceutical sharks,’ Labour MP Graham Stringer said.
The debate in the House of Commons also saw MPs call for the MHRA to be given the power to demand all safety and trial data from pharmaceutical companies.
MPs also heard British pharmaceutical company GSK (GlaxoSmithKline) had held back test results that linked the antidepressant paroxetine to an increased risk of child suicide.
MPs were also told the Yellow Card reporting system, which asks doctors and pateients to report side effects of drugs, was not fit for purpose.
Sharon Hodgson, the Labour MP for Washington and Gateshead South called the system ‘broken’.
An MHRA spokesperson said: ‘We listened closely to the debate. We will now reflect carefully on the opportunities to improve our performance in several areas, including our efforts to fully embed the patient voice throughout all our regulatory activities as we strive to be a more inclusive and transparent regulator.
‘The minister’s full response can be read on Hansard.’
https://hansard.parliament.uk/Commons/2025-01-16/debates/4BF8018B-9662-427B-A580-2EBB7770D164/MedicinesAndHealthcareProductsRegulatoryAgency?highlight=danny%20kruger#contribution-864E4582-C82D-4F1B-9CB3-3397C67FD124
Esther McVey
The number of people who have taken their lives after coming off SSRIs shows that it is not a one-off or rare. There are many people, including one of my constituents, aged only 25, who took her life. I congratulate my hon. Friend on raising this issue. What more can we do to raise awareness of the effects of withdrawal from these antidepressants?
Danny Kruger
The tragedies that we read and hear about are bringing to light the chronic problem of over-prescription in our society. I am afraid that the MHRA is to blame. A review is under way, but it does not sufficiently recognise the direct harms that these pills can induce in people. I hope that through better labelling and regulation, and a better culture of alternative prescriptions, we can reduce the tragedies that we are so familiar with.
‘I welcome the MHRA’s new chair, Professor Anthony Harnden, who was appointed at the start of the year. I hope he is listening to this debate, as it will be important for him in setting his priorities.’
These comments indicate how poorly those who think they are trying to help understand the system they claim to be trying to fix. The MHRA are responsible for nothing – they are a bureaucracy who are responsible only for a paper trail and likely keep a pretty good paper-trail
D
I don’t hold the UK regulatory authority reponsible. They are deli.vering bureaucratically within a commerically constructed and dominated system – that has gone virtually unchallenged by medical professionals, medical journals and, until recently, politicians. Harmed patients – and the few who support them – have been the only real voces of dissent. But, the pharmacovigilancce function the regulators oversee – useless as it now is in terms of under-reporting, coding imprecison etc. – surely has some potential to challenge the system? In the same way the Rxisk ProForma has the potential to challenge prescribers to listen to their patients..
From Dr Peter Gordon
I have submitted the following rapid response and hope that the BMJ
will publish it:
Dear Editor
Suicide and prescribed SSRIs: missed opportunities
In order to prevent future deaths it is vital that collective action
is taken. National Suicide Prevention strategies [1], Royal Colleges,
NICE, MHRA, medical journals and mental health charities need to work
together to ensure prescribers and patients are fully aware that
suicidality and impulsivity can arise when starting, changing or
stopping SSRI antidepressants.
Baroness Cumberlege began the ‘First Do No harm’ report by stating “We
have found that the healthcare system is disjointed, siloed,
unresponsive and defensive” [2]
The First Do No harm review was published in 2020. Yet, to my
knowledge, there have been very few formal responses from within the
healthcare system to this review. Indeed, in asking about this, I have
found that many healthcare professionals have responded: “Cumberlege
what?”
Drug induced akathisia has long been recognised [3]. Lives could be
saved if there were structured and regular formal education about this
issue along with the provision of services as suggested by Dr Peter
Selley [4]. Yet, a recent ‘Practice Pointer’ Assessment and management
of self-harm and suicide risk in young people, published by the BMJ,
omitted to mention consideration of drug induced akathisia as a risk
factor [5].
In Scotland, nearly 1 in 4 adults are taking prescribed
antidepressants, and most commonly beyond the period of treatment
recommended in national guidelines. In 2021, my wife wrote to the
British Journal of General Practice about antidepressant prescribing
[6]. She said “This is important now” and continued “there are large
numbers of people who need help in coming off their medications”,
concluding “General practice, and the RCGP in particular needs to
resist the urge to defensiveness, learn the lessons of experience and
show leadership in addressing this problem.”
Collective action is required now. Missed opportunities mean that
avoidable deaths will continue to happen.
TheBMJ encourages responses from anybody with something relevant to share , including from lay people . Only three responses have been published so far ….there just insn’t a swell of interest from doctors even yet
This is close to a complete and outright lie. Encourages responses which it then refuses to publish if they deal with adverse events. Doctors have learnt not to respond unless they are saying treatments are great and everyone should be on more and more
D
Maybe it’s time to get away from the medical publishers and hunt down a good listening ear elsewhere – aha! Samizdat Health of course! Is there any possibility that Samizdat would be able to publish articles of information plus comments based on the articles as well as stories from those who have been harmed plus those who have been “saved” from the depths of despair by different means? Money would obviously need to be raised to cover the costs – is it time to put money where our mouth is in order to provide literature that we feel would be of great importance, to be shared, for example, in our localities?
Talking to people about these matters is good – but sharing in print could be great. Such a wealth of information that we have here and on Rxisk is seen by relatively few of those who really need to start believing what is going on and how things could change if we had their support.
Is it worth a try?
Mary
Its not just money to make something. It’s having a distribution channel – this is what pharma has – the have BMJ, NEJM. BBC, ABC, CBC, CNN – it’s not possible to compete
D
Duplicitous Serenity.
Sometimes, a person’s existence is commanded by the vice grip of adverse drug effects.
They proceed in traps of turmoil and being conflicted: withdrawal proved unconscionable, but walls of tolerance continue looming cruelly.
They might fleetingly wonder why they took those pills in the very first place, and again repeatedly over all of those initial yesterdays, as those days turned into weeks, then became months, and culminated in years.
Naturally, reasons and justification abounded.
It was not their fault that they were subject, in and out the house, to nonstop pressure! Balance the books! House! Car! Job! Colleagues! Research! Foreign Holidays! School fees! Religion! Panic at the Claustrophobic Church! Marriage! In-Laws! Family! Friends! Neighbours! Restrictions on Alcohol!
They were entitled to relax, surely. They had studied and worked so hard for so very long.
They would easily fight off the pills’ paltry dominance … when the time became right …but all their happiness vanished …
Dear Dr. David Healy, Dr. Pedro and others. . All psychiatric drugs such as SSRI should be banned. None of the psychiatric drugs can or do improve mental health. The reason for this is that the mind and mental illnesses are in the soul (not in the brain). The mind and mental illnesses are not in the brain. They are in the soul. Therefore, psychiatric drugs cannot treat mental illnesses. The best thing psychiatric drugs do is to damage people’s brains. In other words, psychiatric drugs cause permanent brain damage caused by chemicals (usually in the long term; months / years) and permanent mental illnesses related to this. Not only in the long term. Sometimes, it can happen in the short term (immediately / days / weeks later) in people with weak constitutions. I have a terrible prediction. I am concerned that millions of people worldwide have suffered permanent chemical brain damage and possibly related mental illnesses due to this feature of psychiatric drugs. This chemical brain damage cannot be detected by any medical testing tools (MRI, X-ray, blood, etc. laboratory tests). The fact that it cannot be detected is something that suits the psychiatry and pharmaceutical industries. This allows psychiatric drugs to be prescribed to everyone. This situation causes millions of people worldwide who use psychiatric drugs to suffer permanent brain damage and possibly related mental illnesses due to the chemicals that cannot be detected. In summary. . Psychiatric drugs make natural psychological problems permanent. Therefore. . All psychiatric drugs such as SSRI should be banned. In the treatment of mental illnesses, drug-free behavioral therapy and treatment methods should be used. Sincerelly. Thank you..
I doubt if you will get much support for this view particularly among younger women who for whatever reason are taking these drugs more and more. You have made an argument that based on your beliefs you should never have a psychotropic drug – and perhaps not be forced to have one. But you cannot say what others should do. Most of us find a range of meds acting on our nervous systems from tea and coffee to nicotine alcohol and SSRIs can have useful ‘mental’ effects. A lot of us have given up on the idea of a soul as you outline it. I’m not clear how behavioural or other non-drug therapies would work on a soul of this sort any more than drugs would
D
You state that “permanent brain damage caused by chemicals can happen even in the short term in people “with weak constitutions”. I beg to differ. Meeting with many who are stuck in withdrawal from these drugs and hearing of their suffering shows me that they are some of the ones with the STRONGEST constitutions on this earth! The suffering, both on and in coming off these drugs is beyond words. Having watched a loved one, tortured by his ‘medication’ taken on trust, I can only say that those of “a weak constitution” would have caved in many months ago!
It would be interesting to find out if all sufferers of this nature DO have something in common, maybe genetically – in which case each person could be tested prior to being put on the drug but that is unlikely to happen, of course, as it could mean less drugs being handed out!
For the record – this (second attempt) Rapid Response was submitted by me to BMJ on Tuesday 21st.
So far it seems that it is not going to be published:
——————————————————————————————————————
Status message from BMJ 11.55 21 Jan 2025
eLetters Re: Urgent need for review of Guidance and education for prescribers has been created
——————————————————————————————————————-
Urgent need for review of Guidance and education for prescribers
Dear Editor
Please may I comment on Clare Dyers’ BMJ News article 13 January 2025 (1) covering the widely-reported national news of the Coroner, Katy Skerrett’s, ‘Prevention of Future Deaths’ report in the sad case of the suicide Thomas Kingston.
“Katy Skerrett, senior coroner for Gloucestershire, has sent a regulation 28 report, intended to prevent future deaths, to the National Institute for Health and Care Excellence (NICE), the Medicines and Healthcare Products Regulatory Agency (MHRA), and the Royal College of General Practitioners.”
Importantly “The inquest heard that the drugs had been prescribed in accordance with NICE guidelines.”(1)
I refer to the responses that were published by the BMJ to the August 2024 ‘BMJ Practice Pointer’ article on the topic of self-harm and suicide (2). In particular, The BMJ Editors’ response on 25 November 2024 stated that “Adverse effects of medication were not the focus of this education article”.(2)
There is a section in the NICE NG225 entitled ‘Recommendations for safer prescribing and dispensing’ (3) – also reflected in the BMJ Practice Pointer (2) – where known adverse prescribed drug (ADR) effects (including risks of self-harm and suicide) ARE NOT INCLUDED.
With the high publicity surrounding the Kingston case, there is growing public awareness of the medication-related issues related to self-harm and suicide and growing clear evidence of what is actually happening ‘in real life’ – to ourselves, loved-ones, friends, and colleagues. Katy Skerrett’s report offers an unprecedented and clear opportunity for a radical review and urgent updating of NICE guidance, GP/prescriber education and MHRA ADR reporting – to enable the early recognition and management of adverse drug effects, thereby preventing countless future such suicides..
BMJ can hopefully play a very important part in this too, with its global educational reach.
Thank you Marion
“…in accordance with NICE guidelines”
The source for this mantra seems to be the Guardian newspaper coverage
https://www.theguardian.com/uk-news/2025/jan/10/coroner-issues-warning-about-antidepressants-after-suicide-of-royals-husband
“The inquest heard that the antidepressants prescribed to Kingston by his doctor were in accordance with Nice guidelines.”
Who gave this evidence?
Which NICE guidelines are they referring to?
A diagnosis must have been established before any treatment was commenced.
The two separate NICE guidelines for managing Depression and Generalised Anxiety Disorder are so long-winded that they are impossible to follow to the letter.
p.s.
BMJ has been caught with its knickers down over this
BMJ has now published more of our respective Rapid Responses:
https://www.bmj.com/content/388/bmj.r67/rapid-responses
They are really great all of them. Put together some that really hit it for myself:
The terror, intensity of agitation and vulnerability to self harm, combined with inability of the sufferer to explain what is happening to them may lead to misdiagnosis.”
“Immediate prescriber recognition may also prevent incorrect diagnosis (eg psychotic depression) and inappropriate psychiatric detention with enforced use of psychotropic drugs which intensify the toxic state, and increase the risk of self harm and/or violence.”
“Despite that the term was coined more than a century ago, awareness of akathisia’s causes, symptoms, and management remains alarmingly low among healthcare professionals. Given that this medication-induced disorder can precipitate self-harm, suicide, and violence, this knowledge and training gap contributes to avoidable tragedies that could be prevented. (Your recent article regarding self-harm reduction among young people did not mention akathisia as a risk factor.)
To uphold the medical oath to “Do No Harm,” it is essential that practitioners understand the risks and benefits of medications and communicate akathisia information prior to prescribing. It is also imperative that coroners identify and report akathisia-inducing medications in relevant cases. Such information is vital to recognizing when suicides are or might be iatrogenic rather than typical deaths of despair.”
“With the high publicity surrounding the Kingston case, there is growing public awareness of the medication-related issues related to self-harm and suicide and growing clear evidence of what is actually happening ‘in real life’ – to ourselves, loved-ones, friends, and colleagues. Katy Skerrett’s report offers an unprecedented and clear opportunity for a radical review and urgent updating of NICE guidance, GP/prescriber education and MHRA ADR reporting – to enable the early recognition and management of adverse drug effects, thereby preventing countless future such suicides.”
“Drug induced akathisia has long been recognised [3]. Lives could be saved if there were structured and regular formal education about this issue along with the provision of services as suggested by Dr Peter Selley [4]. Yet, a recent ‘Practice Pointer’ Assessment and management of self-harm and suicide risk in young people, published by the BMJ, omitted to mention consideration of drug induced akathisia as a risk factor [5].
In Scotland, nearly 1 in 4 adults are taking prescribed antidepressants, and most commonly beyond the period of treatment recommended in national guidelines. In 2021, my wife wrote to the British Journal of General Practice about antidepressant prescribing [6]. She said “This is important now” and continued “there are large numbers of people who need help in coming off their medications”, concluding “General practice, and the RCGP in particular needs to resist the urge to defensiveness, learn the lessons of experience and show leadership in addressing this problem.”
Collective action is required now. Missed opportunities mean that avoidable deaths will continue to happen.”
“Establishing educational programmes on Akathisia recognition and management for clinicians and organisations e.g. NHS 111 and Samaritans.
Provision of a 24 hr SSRI helpline staffed by clinicians.
Patients prescribed SSRIs for the first time should be given an information leaflet explaining risks, especially of Akathisia, and when to call the helpline.*
The patient information leaflets should be modified to be clearer about what to do if adverse events occur and when to call the helpline.
* There is a precedent: The MHRA recently produced a Risk Acknowledgement Form which is mandatory for certain patients taking valproate.”
Chris
This comment and the previous one from you is a great illustration of a point made by Karl Kraus – a critic of Freud who said some wonderful things. He said people worry about the cure being worse that the disease but there is one cure that has become the disease. Psychoanalysis is the mental illness that it claims to cure.
What you describe here and in previously fits the bill perfectly. Sad to say – its been obvious for 3 decades that psychopharmacology was fast becoming the disorder it claims to cure.
David
NHS Key Facts about Sertraline
https://www.nhs.uk/medicines/sertraline/about-sertraline/
Stark warning – eating grapefruit whilst taking sertraline is dangerous.
The Good News for the Modern Man or Woman:
“Sertraline will not change your personality, it will simply help you feel like yourself again.”
Simples
(page due to be reviewed on 2nd February 2025)
“Sertraline will not change your personality, it will simply help you feel like yourself again.”
I had two 50mg tablets of sertraline and 10 years of my life were destroyed in the most horrific way. I have permanent physical disability
And am socially shunned as a direct result of akathisia not been recognised and even when it was by myself and I repeatedly said this to psychiatrists and nurses my doing that was seen as part of my “illness”.
Chris
This comment and the one from you that follows is a great illustration of a point made by Karl Kraus – a critic of Freud who said some wonderful things. He said people worry about the cure being worse that the disease but there is one cure that has become the disease. Psychoanalysis is the mental illness that it claims to cure.
What you describe here and in the following comment fits the bill perfectly. Sad to say – its been obvious for 3 decades that psychopharmacology was fast becoming the disorder it claims to cure.
I’m going to repeat this comment after your next one –
D
From Ron Law, Risk and Policy Advisor New Zealand
What’s telling is the plethora of retired medical practitioners responding.
Does this reflect a lack of knowledge/understanding on the part of younger practicing practitioners, or just the fact that being retired they can speak out knowing that they won’t be disciplined or ‘cancelled’ or demonised or ostracised or defunded or all of the above?
Hat’s off to Pedro and all who’ve contributed insightful responses, experiences and actions to create awareness and, most importantly, fuel systemic change to reduce this avoidable harm and death.
Marion, your Rapid Response to the BMJ article about harm reduction among young people was excellent and we might submit another one on behalf of MISSD. Today they published our response to the recent coroner’s article here: https://www.bmj.com/content/388/bmj.r67/rapid-responses
British Journal of General Practice
Intended for Healthcare Professionals
Clinical Practice
Withdrawing from SSRI antidepressants: advice for primary care
Emilia G Palmer, Sangeetha Sornalingam, Lisa Page and Maxwell Cooper
British Journal of General Practice 2023; 73 (728): 138-140. DOI: https://doi.org/10.3399/bjgp23X732273
Published eLetters
Withdrawing from SSRI antidepressants
Susanne Stevens
Learning from experience
Peter J. Gordon
A step change in guidance on withdrawing antidepressants
Mark A. Horowitz
Withdrawing from SSRI antidepressants – practical help is needed
James Moore
Withdrawing from SSRI antidepressants: advice for primary care
Greg Butler
Managing withdrawal symptoms using tapering strips
Peter C. Groot and Jim van Os
Withdrawing from SSRI antidepressants: advice for primary care
Dr. Timothy R. Moss. FRCGP.
Withdrawing from SSRI antidepressants: advice for primary care
Cathy Wield
Withdrawing from SSRI antidepressants
Susanne Stevens, retired social scientist, n/a
There needs to be some serious questioning as to why the condition of akathisia is missing from the article’s contents. It is a proven life changing condition which causes such distress some commit suicide. So why the silence? The general public cannot rely on campaigning groups to inform them – only a relatively small number of people are aware of them and then only become aware when bereft of help from health workers they turn to campaign groups i.e. when the situation is already dire. This month January 25 there is yet another attempt by the same people to highlight the issue – when will anything change unless journals do their bit more than simply publish these articles.
Withdrawing from SSRI antidepressants: advice for primary care
• Greg Butler, Salaried GP, Senior Medical Officer, Ministry of Defence, MoD Stafford.
“My lived-in experience has shown many patients simple stop SSRIs outside medical recommendation with minimal reported side effects so perhaps we are exaggerating withdrawal issues.”
“If we recall, Prozac was the first SSRI of use and all others that followed were “me-to” products of Big Pharma, merely developed to get a slice of the significant financial action. Logically they have no tangible benefit over fluoxetine, all working on the same 5 HT pathway. So, therefore, fluoxetine should be considered the drug of choice?”
I guess he might have prescribed a lot of Prozac everybody. Do you think he knows that the person who was tasked with promoting and bringing Prozac to market became a whistleblower clearly stating that in a small trial within the first week, two of the patients tried to commit suicide. He goes on to name the condition:
AKATHISIA
7mins in
https://www.youtube.com/watch?v=9Eet4x5_8tE
Re: Coroner questions advice on risk of suicide with SSRIs after death of financier Clare Dyer. 388:doi 10.1136/bmj.r67
Dear Editor
The recent article highlighting the coroner’s concerns about the link between SSRIs and suicide is a critical reminder of the often-overlooked questions that need to be asked after such tragedies. I know this all too well. If it weren’t for the Minneapolis coroner asking me whether my husband, Woody, was on any medication, I might never have known that sertraline—the antidepressant he was prescribed by his family doctor for insomnia—could have played a role in his sudden and shocking suicide. Woody wasn’t depressed nor did he have any history of depression and had been on sertraline for just five short weeks before he was found hanging. That single, simple question from the coroner sparked what would become a lifelong drug safety advocacy effort, including helping to secure FDA black box warnings on antidepressants for the increased risk of suicidal thoughts and behaviors in 2004 and 2006.
This experience taught me that coroners, as frontline investigators, play an essential role in uncovering potential drug-related harms. Yet their observations are too often dismissed as mere “anecdotes.” When my family met with top FDA officials—along with other families who had lost loved ones to antidepressant-induced suicide—we were told these deaths were “just anecdotes,” not meaningful data. But anecdotes are data points. Each life lost represents a real-world outcome that deserves investigation and acknowledgment.
Why aren’t we asking the right questions after every suicide or mass shooting? Was the individual prescribed an SSRI or other psychotropic medication? What was the timeline of events leading up to the tragedy? Without gathering and analyzing these data points, we are missing a crucial opportunity to uncover patterns that could save lives. Tragically, when we approached coroner offices to encourage the tracking of SSRI use in cases of suicide and mass shootings, we were met with resistance, often under the guise of HIPAA concerns. This systemic resistance leaves dangerous gaps in our understanding of how these drugs may contribute to preventable deaths.
I commend Gloucestershire’s senior coroner, Katy Skerrett, for issuing a regulation 28 report to NICE and the Medicines and Healthcare Products Regulatory Agency. Her actions highlight the need for a shift toward more robust postmortem investigations into the role medications play in suicides.
Twenty-one years ago, the Minneapolis coroner’s decision to take Woody’s sertraline bottle with her was the pivotal moment that led me to the truth about his death. It was a moment of curiosity that lit a fire under my family to demand answers and create change. If every coroner were empowered to ask these questions and document findings related to SSRI use, we could build a body of evidence that regulators, healthcare providers, and the public could no longer ignore.
I urge coroners everywhere to recognize their unique role in identifying these “hidden” patterns of harm. By being curious, asking questions, and documenting medication use in cases of suicide or sudden violence, they could help shine a light on the risks associated with SSRIs and other medications. These are not just anecdotes—they are lives lost, and their stories must be told.
Kim Witczak
Co-founder Woodymatters, Advisor to MISSD Board of Directors, and FDA Psychopharmacologic Drugs Advisory Committee Member
Competing interests: No competin
Google any news outlet and this is reported all around the country. Coll of Psych’s response is a disgrace
BBC News
Published
4 February 2025, 06:00 GMT
Updated 1 hour ago
The parents of Thomas Kingston, the husband of Prince and Princess Michael of Kent’s daughter, have warned about the side effects of antidepressants after he took his own life.
Mr Kingston, who was married to Lady Gabriella Kingston, the King’s second cousin, died from a head injury in February last year at his parents’ home in the Cotswolds. A gun was found near his body.
The 45-year-old had stopped taking his medication, which had been prescribed by a GP at the Royal Mews Surgery – a surgery for Royal Household staff in Buckingham Palace – in the days leading up to his death.
His parents, Martin and Jill Kingston, are now calling for a change in how patients are prescribed selective serotonin reuptake inhibitors (SSRI) – a widely used type of antidepressant.
Martin Kingston told BBC Radio 4’s Today programme he believes both the patient and the people close to them should be told more explicitly about the potential side effects of the medication, including what can happen if they stop taking it.
The couple want patients to sign a document confirming they’ve been told about the difficulties of going on and coming off the medication. This could include the patient being told that “it’s an extreme case, but it could lead to suicide”, Mrs Kingston says.
“We’d really like to see that a person, a spouse, a partner, a parent, a close friend, somebody, was going to walk with them through it. Maybe they should be at that signing time.”
He says part of the issue is doctors are under pressure to help patients during a typically short appointment slot. He says if a person complained that they were stressed and not sleeping and rejected the GP’s suggestion to try cognitive behavioural therapy, a talking therapy used to help with mental health conditions, the doctor might prescribe an antidepressant out of a “desire to help”.
More than 8.7 million people, external in England were prescribed antidepressants in the 12 months to March 2024, according to the NHS Business Services Authority.
The NHS says, external that SSRIs generally have fewer side effects than most other types of antidepressant and the majority of people will only experience “a few mild side effects”, though some people, external “have suicidal thoughts and a desire to self-harm” when they first take them. It advises patients to tell a relative or close friend that they’ve started taking antidepressants and ask them to say if they’re worried about changes in their behaviour.
When people come off antidepressants, the NHS advises, external they reduce their dose “slowly, normally over several weeks or months”, to prevent withdrawal symptoms, which can include mood changes. The Royal College of Psychiatrists says anyone thinking of stopping antidepressants “talk to their doctor first… [T]hese medications should not be stopped abruptly”.
Mrs Kingston told the Today programme she’s aware of why people take SSRIs. “We have many friends who are on them, and we totally understand why they’re on them at the same time,” she says.
Tom had initially been prescribed sertraline and zopiclone, a sleeping tablet, after complaining of trouble sleeping following stress at work.
After returning to the GP and saying they were not making him feel better, he was moved from sertraline to citalopram, a similar SSRI drug.
He was off the medication at the time of his death and his parents say there was “nothing that raised any suspicions,” though he did have a “strong reaction” to the first SSRI, Mrs Kingston says.
On the day of his death, “he was normal”, she added. “He was fun. We were laughing about various things.” The family spent the day relaxing, reading and sitting by the fire, she says
He describes Tom as a “joyful, giving, full of life and caring person”.
After his death, the family was sent more than 400 cards and letters, he says, adding: “So many of them told us things that we never knew.”
Recording a narrative conclusion at an inquest into his death in December, Katy Skerrett, senior coroner for Gloucestershire, said Thomas Kingston had taken his own life.
“The evidence of his wife, family and business partner all supports his lack of suicidal intent,” she said at the inquest. “He was suffering adverse effects of medication he had recently been prescribed.”
In a prevention of future deaths report, made in January, Ms Skerrett said action must be taken over the risk to patients prescribed SSRIs. She questioned whether there was adequate communication of the risks associated with such medication.
In a statement, the Royal College of Psychiatrists said antidepressants were “highly effective at reducing the symptoms of depression and other conditions such as anxiety and panic disorders, particularly when used in combination with talking therapies.”
“These treatments reduce suicide risk and can save lives,” a spokesman said.
Tom’s parents told the Today programme they hoped that by speaking out they could prevent someone having to experience what they did.
“We wouldn’t be able to be comfortable reading about somebody else going through what we’ve been through, if we had not made clear what we think could happen to save someone’s life and save someone’s grief,” Mr Kingston said.
BBC Today R4 interviewed Thomas Kingston’s parents. After the interview, they would be talking to an expert to discuss this further.
07.32 Jill and Martin Kingston
08.14 Professor Allan Young
https://www.bbc.co.uk/sounds/play/m0027ltn
Jill and Martin Kingston, poignant, brave and with devastating words of clarity ‘leaning in to the pain’, and offering their suggestions to improve the current situation.
The expert psychiatrist, ‘I note that Mr. Kingston had an anxiety disorder – there does seem to be an impulsive nature –
I found this a deeply offensive rebuttal, to the Kingston’s, the Coroner’s Report and the Psychiatric Report, as referenced by Mr. Kingston.
Most Media are covering the story
Parents of Lady Gabriella Windsor’s husband Thomas Kingston break down in tears as they speak for first time since he took his own life to call for new warnings about anti-depressant ‘side effects’
https://www.dailymail.co.uk/news/article-14358017/We-lovely-lunch-fell-asleep-woke-Tom-missing-nightmare-started-Family-Lady-Gabriella-Windsors-husband-speak-time-took-life.html
“The expert psychiatrist, ‘I note that Mr. Kingston had an anxiety disorder – there does seem to be an impulsive nature –
I found this a deeply offensive rebuttal, to the Kingston’s, the Coroner’s Report and the Psychiatric Report, as referenced by Mr. Kingston.”
Absolutely and the RCP use what happened to promote AD’S:
“In a statement, the Royal College of Psychiatrists said antidepressants were “highly effective at reducing the symptoms of depression and other conditions such as anxiety and panic disorders, particularly when used in combination with talking therapies.”
“These treatments reduce suicide risk and can save lives,” a spokesman said.
“Coll of Psych’s response is a disgrace”
Very much so.
It’s going to get much worse and there will be even more draconian measures by the looks.
The expert psychiatrist, ‘I note that Mr. Kingston had an anxiety disorder – there does seem to be an impulsive nature
there does seem to be an impulsive nature
I would describe it as a driven compulsion as a result of a catastrophic internal condition that is not ostensible to others and would be terrifying way way beyond anxiety. But yes AKATHISIA can look to others as being impulsive. However no excuse coming from a esteemed’ psychiatrist.
Recognizing the difference between real anxiety which is what he had before going to the GP to what happened to him after taking sertraline which was AKATHISIA and acting correctly – which for me would be stopping the medication and helping his body initiate GABA plus appropriate sleep videos and counseling for what ever triggered his anxiety in the first place – is where, not just the GP in this case, went wrong but just about every other health care professional and is a major disaster particularly in psychiatric hospitals.
There is no information given as to what happened to the trial participants after the trial ended Even when it is known severe adverse effects may occur in future. The advice given about anti depressants is to take them for several weeks before any any potential benefits kick in – yet this trial was ended for some in 4weeks . Seems a pretty sloppy piece of research which has the potential for expanding the use of SSRIs by claiming short term efficacy which could for many lead to long term use with increased potential for serious adverse effects. It is negligent to use people in trials without following up long term to monitor for known harms
January 30, 2025
expert reaction to Cochrane review of the effectiveness of anti-depressants versus placebo for generalized anxiety disorder
Dr Gemma Lewis, Senior Research Associate in Psychiatric Epidemiology, University College London (UCL), said:
Meta-analyses are often considered the best way of informing guidelines for clinical practice. Importantly, the individual studies were generally of good quality too.
“The authors only included Randomised placebo-controlled trials. This type of study is the best way of evaluating whether a treatment is effective. The randomised design eliminates the possibility of confounding.
“One limitation of the data is that most studies only followed people for up to 12 weeks. In reality, we know that many people use antidepressants for much longer than this, often for several years. In the future, we need trials that follow people for longer periods. Another limitation of the data is that most studies only included people with a clinical diagnosis of anxiety, which is quite severe. In reality, many people are prescribed antidepressants in primary care for milder symptoms of anxiety as milder symptoms can still be debilitating.
“GAD is the most common mental health problem, and it can be very debilitating. However, in research, and also perhaps clinically, it is often neglected, particularly when compared to depression. The antidepressants were generally well accepted by people who used them although some people of course experienced side effects, as is the case with most medications. These findings reinforce the usefulness of antidepressants for treating symptoms of anxiety as well as depression.”
Prof Christiaan Vinkers, Department of Psychiatry and Anatomy and Neurosciences, Amsterdam UMC, said:
“The Cochrane review confirms what science has long shown: antidepressants work for Generalized Anxiety Disorder (GAD), with SSRIs and SNRIs consistently outperforming placebo. Their effects are meaningful, with a low number needed to treat (NNT), and dropout rates are comparable to placebo. However, antidepressants continue to face disproportionate skepticism, whether it is for GAD or depression. If these results were for heart disease or diabetes treatments, they’d be celebrated. Instead, antidepressants are often unfairly stigmatized, fueling misinformation which can deter people from seeking treatment that can have added value. Antidepressants aren’t a cure-all, but they are an essential, effective tool. Let’s shift the narrative from fear to facts: science should guide treatment, not stigma.”
Prof Katharina Domschke, Department of Psychiatry and Psychotherapy, University of Freiburg, Germany, said:
“This is a comprehensive, long awaited update on the efficacy of antidepressants versus placebo in generalized anxiety disorder (GAD).
“SSRIs and SNRIs, the first line treatment options for anxiety disorders according to all international guidelines, were shown to have a significant benefit of a placebo.
“The study is methodologically strong, applied a conservative outcome measure (greater than 50% reduction in Hamilton Anxiety score), excluded regular benzodiazepine use and controlled for study quality.
“Limitations of the present study comprise its limitation to adult patients and the wide range of treatment duration (4 to 28 weeks).
“Interestingly and importantly, no difference in overall acceptability was discerned between antidepressants and placebo.
“The present results are very important and ought to increase patients’ trust in the efficacy of pharmacological treatment of GAD. “
But Prof Peter Tyrer, Professor of Community Psychiatry, Imperial College London, happily retired and so more at liberty to speak without anxiety says;-
“The findings of this review are unequivocal – antidepressants are effective in the treatment of generalised anxiety in the short-term. But in responding to this evidence the long-term implications have to be considered also. Here the conclusions of efficacy have to be tempered. Long-term treatment, as noted in the review, is often the norm, and there is increasing concern that patients have difficulties in stopping antidepressants because of withdrawal problems. Bearing in mind that the main reason why antidepressants were preferred to benzodiazepines (drugs that are equally effective in treating generalised anxiety) was the dependence risk, we just seem to have shifted the problem of adverse effects from one class of drugs to another. Brief resolution does not effect a cure”
Cochrane
One of the primary authors states here that the trials ran for 4-12 weeks not 4 – 28 weeks as stated by K.D. above.
‘Antidepressants versus placebo for generalised anxiety disorder’ by Kopcalic et al. was published in Cochrane Database of Systematic Reviews at 01:00 UK time on Thursday 30th January 2025
DOI: 10.1002.14651858.CD012942.pub2
…
Antidepressants reduce anxiety, but long-term impact remains unclear
A new Cochrane review confirms that antidepressants effectively reduce symptoms of generalized anxiety disorder (GAD) under trial conditions, although there is limited data on long-term usage.
The review also highlights the lack of data on the long-term effects of antidepressants. Most included trials lasted between 4 to 12 weeks, with no long-term follow-up.
“We don’t have enough information on the potential long-term benefits and harms of antidepressants, even though people often take them for years,” says first author Katarina Kopcalic, who conducted the review at Western University. “This is an area that needs further exploration in future trials.”
Despite these limitations, the review delivers a clear message: antidepressants are effective for managing GAD, particularly for patients who do not respond well to non-pharmacological treatments. However, more independent, long-term research is needed to understand their full impact, especially in patients with multiple conditions.
Results showed that antidepressants were more effective than placebo in reducing anxiety symptoms, with a 41% higher response rate among those taking the medication compared to those taking a placebo. The review found no significant difference in dropout rates between those taking antidepressants and those taking a placebo, indicating that these medications are generally well-tolerated.
“We don’t have enough evidence to say how effective they may be in patients with GAD alongside other mental health conditions, which is much more common in clinical practice. Most of the patients I see with GAD also have other mental health conditions, so future trials should investigate the effects of different treatment strategies on patients with multiple conditions.”
The review also highlights the lack of data on the long-term effects of antidepressants.
“We don’t have enough information on the potential long-term benefits and harms of antidepressants, even though people often take them for years,” says first author Katarina Kopcalic, who conducted the review at Western University. “This is an area that needs further exploration in future trials.”
The most appropriate comment here is that Tom Kingston’s doctor, Dr Morgan, thought he was suffering from Anxiety.
D
I have recently written to Katie Skerrit, copying Julie Bentley in, Samaritans. Parliament does not respond to a well reasoned academic argument, it responds to pressure. Unfortunately, in the words of Mr Bates v The Post Office …….. “To them, we’re just skint little people.” How long will Pharma be allowed to continue culling our children.