This talk was given in Maastricht at the invitation of David Linden, Scientific Director of the Mental Health and Neuroscience Research Institute on November 27 and again to a group of Primary Care Doctors in Sweden at the invitation of André Marx on Nov 28. There were some great questions afterwards. This post gives the text of the talk along with the slides and links to related posts. There is a video of the talk below but so much more in the text including the outline of a new condition Narcissistic Doctor Disorder than in the live talk.
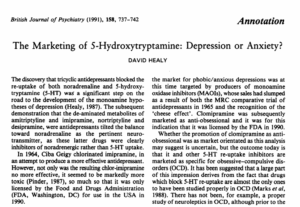
Slide 1. In 1958, Imipramine (in the middle above) was the first tricyclic antidepressant (TCA). By 1959, European psychiatrists, semi-Freudian mostly, agreed it could replace ECT in the treatment of melancholia. But even in these severely ill, often suicidal, patients, doctors could spot imipramine causing suicide. Doctors today can’t spot SSRIs causing suicidality in mild non-suicidal depressions. Why not?
Frank Ayd discovered Amitriptyline’s benefits in melancholia in 1959, which meant he wouldn’t have to continue giving his father ECT on the kitchen table. Melancholia kills libido and Ayd had no wish to create treatment hesitancy but he said amitriptyline caused a sexual dysfunction distinguishable from the effects of melancholia on sex. Doctors can’t now spot SSRIs causing even clearer sexual effects in patients with no prior libido problems. Why not?
By 1961 Julius Axelrod had established the 3 drugs on top here all inhibited norepinephrine reuptake, for which he won a Nobel Prize. This gave rise to Schildkraut’s Catecholamine Hypothesis, the original low neurotransmitter or chemical imbalance hypothesis.
Slide 2. Was melancholia a deficiency disorder like Parkinson’s disease? Would a pure norepinephrine reuptake inhibitor be more effective and free of terrible anticholinergic side effects? There was a snag. Benzodiazepines immediately did something clearly helpful. Ditto antipsychotics and stimulants. But tricyclics seemingly had lots of immediate side effects but no beneficial effect and catecholamine reuptake inhibition was immediate.
Slide 3. This is what melancholia, a disorder of middle or older years, looked like then. After 2 weeks treatment with ECT or TCAs it showed a response. But if there was no immediate and obvious drug effect, what was driving this? Did the drugs cure a lesion?
Slide 4. Fridolin Sulser’s catecholamine receptor hypothesis took over. These proteins might need chiseling for two weeks to come right. We now know receptors respond almost instantly but the weeks of chiseling notion legitimized the idea that TCAs took 2 weeks to correct a lesion. Like the Cheshire Cat, Sulser’s Receptors and then BDNF Biobabble left a Grin behind – we have to wait up to 6 weeks now for something to happen, even for much milder problems than melancholia, before people get well. In the meantime. they just have to put up with side effects.
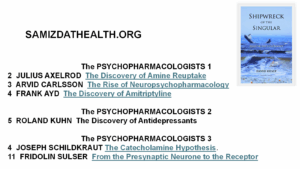
Slide 5. I have over 100 interviews with early psychopharmacologists including Axelrod, Ayd, Kuhn, Schildkraut, Sulser and Carlsson. It costs over $1000 to buy the books these are in, but you can download all interviews for free from the Samizdathealth.org website, linked to Shipwreck of the Singular – See Shipwreck The Psychopharmacologists. Email me if you can’t find them.
Slide 6. All of the TCAs here except trimipramine inhibit norepinephrine reuptake. But in the 1960s psycho-analysts claimed Imipramine, Amitriptyline and Clomipramine had an impact on transference reactions which desipramine didn’t have. The impact was immediate.
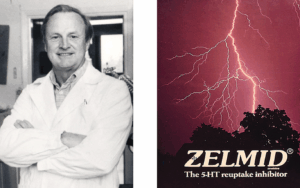
Slide 7. Listening to this, Arvid Carlsson linked the changes in transference reactions to serotonin reuptake inhibition – desipramine doesn’t. He made a dedicated serotonin reuptake inhibitor to explore this further – Zelmid. This and later SSRIs mute sensory/emotional reactivity – they are Serenic – Anxiolytic.
Slide 8. Zelmid was not an anti-melancholic drug, it and later SSRIs are Serenics. But it became an antidepressant even though anxiolysis is where the money is because it was almost impossible at the time for a new anxiolytic to compete with benzodiazepines.
Slide 9. It was obvious 35 years ago that SSRI Marketing needed to shape-shift Valium cases into cases of Prozac, cases of anxiety into depression. Companies platformed doctors claiming depression lay behind many cases of anxiety and treating it would offer a real cure not a drug crutch – besides which antidepressants didn’t cause dependence.
Slide 10: For Carlsson SSRIs were a Therapeutic Principle that allow us to compensate for a problem. They were not Magic Bullets that fixed a lesion. Like LSD, working on a normal serotonin system, SSRIs could cause good and bad trips. Bad enough to cause suicide? Yes.
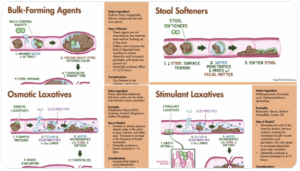
What’s a Therapeutic Principle? There are 4 kinds of constipation and 4 laxative principles. You can add fluid or bulk, stimulate or relax the gut. The wrong principle for your constipation can make things worse. But a company licensed to use the word Laxative would prefer you to be on 4 laxatives provided one is theirs rather than the right one for you. This way treatment resistant constipation lies.
Most medical problems from hypertension to type 2 diabetes, pain, and nervous problems have several potential therapeutic principles – getting it wrong can create treatment resistance. Euthanasia increasingly is the only way out of SSRI induced treatment resistance.
Slide 11. You might expect Therapeutic Principles for nervous problems to act on the brain, but benzodiazepines relax muscles, and beta-blockers slow heart rates, which fools our brains into thinking we are not anxious. But beta-blockers can increase heart rates for some creating anxiety. At this point we need someone who is working with us rather than from a book.
Slide 12. Therapeutic principles ask us to adjust a function to compensate for a lesion not correct it. Walter Hess, a 1949 Nobel Prize winner, directing his male students to think of functions asked them what their work could reveal about why they fell in love with a girl.
They were all guys back then. The girls were using anticholinergic drops to dilate their pupils which left guys thinking a girl liked them causing them to fall in love with her.
Slide 13. What function do SSRI work on? In 9 out of 10 of us, SSRIs cause genital numbing within 30 minutes of a first pill, at a fraction of the antidepressants dose. The degree of genital numbing correlates closely with reports of reduced emotional reactivity. Reduced sensory reactivity has face validity as a therapeutic principle in nervous disorders – and SSRIs work better for anxiety disorders than for depression and don’t work for melancholia.
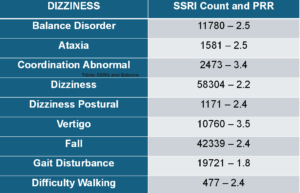
Slide 14. In healthy volunteer trials, dizziness and balance effects are relatively immediate on starting and stopping SSRIs. These are not Side Effects. Balance and touch are sensory effects and show the core action of SSRIs are their sensory effects.
This slide shows balance problems reported to FDA on SSRIs. Only 1 in 100 get reported, so SSRIs have significant effects on our sense of balance for millions of us. PRRs (Proportional Reporting Rates) measure the rate this problem is reported compared to all problems on this drug balanced against the rate this problem is reported on all drugs compared to our drug. A PRR over 1.0 indicates a link, over 2.0 a strong link, and higher again points almost to certainty. These are stronger data than you get from RCTs.
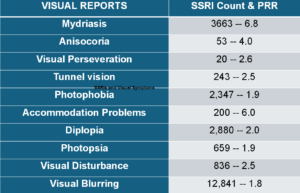
Slide 15. Reports to FDA show visual issues on SSRIs in hundreds of thousands of us. There are less reports to FDA because ophthalmologists don’t report them as you’ll hear.
Slide 16. The idea that an action on sensory functions might be Serenic fits with the James-Lange Theory of the Emotions put forward in the 1880s which said our body senses/feels – it thinks fast – what we call emotions are cognitive interpretations/misinterpretations of these feelings.
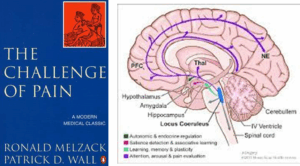
Slide 17. For a century after 1832 when reflexes were first discovered. research established a series of gate controls up through the spinal cord enabling all animals, including us, to function without any mental or spiritual input.
These gates are topped out by a vigilance nucleus – the blue norepinephrine locus coeruleus and the green serotonergic raphe nucleus which damps down vigilance. The locus coeruleus needs the sensory hum to be gate-controlled in order to pick out salient actionable features. The serotonergic Raphe nucleus damps vigilance down. But we can empty out the 5% of serotonin in our brains, which is in the Raphe Nucleus, without causing problems.
Slide 18. I am only semi-saying we don’t need brains at all to work out what SSRIs are doing. I’m trying to get you to see us as more like Octopi than we normally see ourselves. In contrast to appearances, Octopi have Distributed Knowledge Centers in their arms – not in the bulbous head.
Slide 19. Acting on serotonin LSD opens our sensory gates, floods awareness, and overwhelms our heuristic – thinking fast – capabilities. The action on serotonin in humans was shown first in our gut. Very early on spiders, who like octopi have Knowledge Centers in their 8 legs and 8 eyes, given LSD wove weird webs.
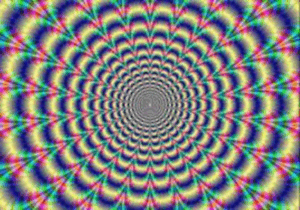
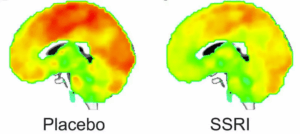
Slide 20. SSRIs mute these sensory gates. This Brain Scan shows the effects of one dose of an SSRI in healthy volunteers – the sensory input from the body is diminished. Sensory Deprivation Tanks do something similar. This muting might seem to make interpretations easier but in practice muting can compromise our interpretations as you will see.
Slide 21. This quote gives you a sense of how sensorily deprived people can be.
The mental state is literally an altered state of consciousness that one absolutely cannot comprehend if he didn’t experience it. No words can explain such a thing. I am shocked such a state is even possible.
The best way to describe it is mental anesthesia. Everything in the mind is tuned down so low, even thoughts, emotions so muted they are barely relevant.
It’s the opposite of what psychedelics do. They enhance and amplify whereas SSRIs completely mute. One has the impression everything has been wiped out and there is no mind anymore.
Slide 22. Just as Cartoonists have known for decades about the biobabble doctors spout, they have also known for decades what SSRIs really do.
Slide 23. Some years ago in this unit we randomized 20 medical and nursing healthy volunteers to a norepinephrine reuptake inhibitor or an SSRI for 2 weeks, then crossed over to the other for 2 weeks. 48 hours into the study a patient asked me if Dr X, who he said was more mellow than usual, was on an SSRI. When we broke the blind – Dr X was on an SSRI. Patients are expert at observing people in a way healthcare staff no longer are.
The Grin of the Catecholamine Cat inhibits our ability to spot the obvious. Uninhibited patients, cartoonists and psychoanalysts see Good or Bad Trips within hours. Two of our volunteers became dangerously suicidal on the SSRI. Becoming suicidal on an SSRI is not a step on the way to an eventual Good Trip.
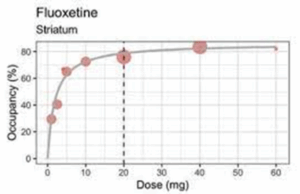
Slide 24. One of the main reasons why SSRIs go wrong is that worried SSRIs might not work in antidepressant licensing studies, as this graph shows companies dosed them at the toxic end of the dose range – 20 mg for Prozac. At 20 mg, a range of problems had to be covered with concurrent benzodiazepines. No trials show SSRIs working on their own.
Giving a benzo would not be a problem in cancer chemotherapy trial because we don’t expect Benzos to be anti-cancer. But using Benzos to damp down agitation in trials of a drug being brought to market to replace hazardous Benzos is perverse.
Looking at this dose response curve. you’d say a 5 mg dose would be optimal. After licensing Lilly published a 5mg Prozac trial. It worked better at a 5 mg dose. It’s lead author Lilly’s Joe Wernicke asked colleagues what do we tell people about this?
Again and again, when someone is not doing well on an SSRI, doctors increase the dose beyond 20 mg rather than lowering it.
Slide 25: Unlike LSD, which we take occasionally and recover from bad trips, we remain on SSRIs for months or years in toxic doses. Unsurprisingly, things break – sensory things break. PSSD (Post-SSRI Sexual Dysfunction), which can last for the rest of your life, points to the profound effects broken sensation can have – see PSSD Podcast .
Bryn: Getting PSSD undermines your faith in the whole system of science as we have it – its not some vague feeling. Losing your libido is equivalent to going blind or deaf, its that level of sensory impairment
Roy: The same can be said for losing your emotions – I felt I lost two senses – my sexuality and my emotions
Bryn: If we want to be believed we have to remember how incredible our story sounds … My Dad says its not possible a drug could cause these effects, it wouldn’t be on the market
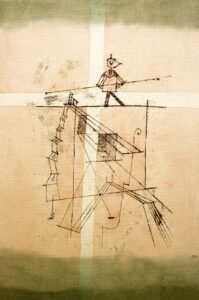
Slide 26. A decade ago criteria for a new syndrome Persisting Postural Perceptual Dizziness (PPPD) were put on the map. This dizziness involves vestibular, visual and proprioceptive input – all of which have a serotonergic component. See Balancing our Bodies and our Selves.
Vertigo is a better word for this. For a tightrope walker vertigo would trigger a panic attack and panic is common in people with PPPD. Both starting and stopping an SSRI can cause PPPD and like PSSD or akathisia PPPD can endure for years. Vestibular Rehabilitation Therapy can help but while waiting folk get referred for trauma therapy and get given SSRIs.
This is not just a matter of negotiating things like climbing some steps, we live on a tightrope and our senses our emotions disturb our internal balance. Sensory disturbances like these strike at the very heart of us and fuel a turn to medical assistance in dying.
Slide 27. This fabulous image brings home a key point that disrupting embodied knowledge. as in VSS and PPPD has profound effects beyond just sensory issues. We’ve just published the largest series of cases of VSS linked to one drug group – SSRIs. Like PSSD, PPPD, VSS can start on starting or stopping SSRIs and can endure for years afterwards and people often figure they are going mad – especially with the response they get from health systems.
See Juggling Our Selves and Our Bodies.
Slide 28. Ophthalmologists and others looking into our eyes and not seeing a lesion, tell people this is a brain or mind problem – made easier to say of course if the person is on or has been on an SSRI. They may babble about thalamo-cortical dysrhythmia – a neuro equivalent to chemical imbalance. The patient gets referred for trauma therapy or has an SSRI recommended.
But comparatively speaking there is more serotonin in our eyes relative to their size than there is in our brains.
Slide 29. SSRIs achieve the effects we want by acting on our primary knowledge generators – our sensory systems. In the toxic doses prescribed they disrupt embodied knowledge. When this happens, patients complain about Brain Fog. They are certain their brains are broken but cognitive tests don’t show this.
When embodied knowledge breaks, we try to fix it by attending or concentrating more which is effortful and frustrating because that’s not the way to repair embodied knowledge – a complaint of Brain Fog almost proves the point.
Slide 30. Embodied knowledge gets made and repaired by blunt repetition. Trying to instruct bodies doesn’t work. The enduring sensory problems after SSRIs explain why withdrawal is so difficult. There is linked damage that does not go away with tapering.
Slide 31. In 1992, I chaired a UK launch meeting for Sertraline – Zoloft – for Pfizer. I told the audience serotonin was more primitive than estrogens or androgens and drugs acting on it would produce effects we had never seen before – good and bad. Science is about paying heed to new observations like these – even bad effects can open the door to new drugs.
You also need to know small molecules are promiscuous – they may have 100 effects. If you want precision you need a big, fat protein. Julius Axelrod who rediscovered acetaminophen – paracetamol, often said serotonin was a relic of our marine past. SSRIs act on something even more primitive than serotonin – they activate carbonic anhydrase enzymes – this produces fluid in confined spaces like our eyeballs giving us glaucoma.
Slide 32: This quote from Bruce Springsteen’s Born to Run captures sensory drivers behind his SSRI linked akathisia.
I was profoundly uncomfortable in my own skin. I just wanted OUT. It feels dangerous and brings plenty of unwanted thoughts. I couldn’t live like this…
I understood what drives people toward the abyss. There was no life here, just an endless irritating existential angst embedded in my bones. It was demanding answers I did not have.
Slide 33. Now adding weird new sensations that need interpreting to sensory muting opens a door, as this person hints, to dominant imagery and the consequences of that.
Just as my vision lost depth – it was more like a 2-dimensional videogame – there was a loss of depth to my thinking. I was reacting to things on the surface rather than able to see through to the consequences.
If I had an impulse to drive, I would go rather than consider the time or whether I had work the next day. If I had an impulse to go out for a walk, I might simply go without my phone – or shoes
Slide 34. Or this woman who ended up in an almost hypnotic state.
I was thinking I wanted to stop, that I didn’t want to do it, but I had to.
Why did you have do it?
Because I had started it – I can’t explain it.
Slide 35. I hope you can see we know what SSRIs do – they mute sensation. We know this from evidence going on them, coming off them, and from the functions they can break in us. Our right hand knows this. Our left hand doesn’t as you will see from Woody Witczak’s case. What happened to Woody has become the norm today.
This is Kim and Woody Witczak. He had just begun a dream job, they were happily married, thinking about a family, had booked trips. After a few nights poor sleep, Woody’s doctor gave him Zoloft. He became agitated. One minute he’d be fine, then lying on the floor saying Kim wouldn’t believe the thoughts he was having. Woody had a good doctor who said this was normal – SSRIs may not start working for 6 weeks. Hang in there. In the fifth week Woody hung himself.
If we are dealing with LSD, we don’t say this Bad Trip you are having will any moment flip over into a Good Trip. Why do we say it about SSRI Bad Trips?
The Grin of the Catecholamine Cat is partly to blame but there is another perverse source.
Slide 36. I’ve doctored the Great Seal of the United States. E Pluribus Unum – from many individuals, one people – now reads Mediocris – the Latin for Average.
Companies do Randomized Controlled Assays (RCAs) mislabeled as RCTs to get products licensed and claim these offer Gold Standard Science on what their drugs do. They brand Evident PSSD, VSS, PPPD, Suicidality or Homicidality as Anecdotes not Evidence.
Like Chat GPT or Grok, RCAs (even RCTs done by angels) are averaging machines. At best they allow us to say this drug is not totally without benefits, but they tell a doctor nothing about how to treat the person in front of them.
The averaging effect means SSRIs don’t differ much from placebos in the mild depression assays they were tested in. Averaging LSD trials would give the same outcome but no-one says this about LSD. The idea SSRIs are nothing more than placebos kills people.
Less than 50% of SSRI trials were positive but, with adverse SSRI effects damped down with benzodiazepines, a bunch of coding and statistical tricks and clear fraud, companies could pull out a result that allowed FDA at 6 weeks to license SSRIs as antidepressants.
These licensing linked maneuvers are the basis to the idea SSRIs may take 6 weeks to work. No lesion clears up. There is no evidence in these trials that a Bad SSRI Trip can finally morph into a Good Trip.
Based on 100,000 patients in company assays, FDA found less than 1 in 6 have a Good Trips on SSRIs. These 1 in 6 Good Trips allowed SSRIs to be licensed as antidepressants.
If companies had sought a license as a Serenic, the trials could have been as short as a week long and would have yielded a marked difference from placebo. Marketing got in the way of this. A Serenic license would have left too much to the discretion of doctors.
There is a further problem with RCTs. Not only do they average good and bad trips on one drug but if LSD and SSRIs and benzodiazepines and stimulants and antipsychotics were all put into trials of mild depressive disorders, although entirely different treatments doing completely different things, they would all end up looking the same – giving the same 3 points difference on a depression rating scale score.
I’m not sure we can blame FDA for this. The drugs have the capacity to work just like they have the capacity to cause suicide. Back around 1990, FDA may have expected doctors to work out how in practice to use these drugs to better effect than company assays suggested.
Slide 37. RCAs allow companies to create a Wonderland. The label attached to their drug acts like the labels Alice faced in Wonderland where food and drink were labeled Eat Me and Drink Me leaving her incapable of not doing this. FDA labels have this effect on sophisticated women who won’t take soft cheeses, or processed meats but consume prescribed SSRIs in ever greater quantities when pregnant.
Freudians who spotted serotonergic impacts on transference reactions can explain what’s going on. Companies have nudged doctors and an educated elite into Delegating Narcissism to FDA .
Slide 38. Mark Anthony said he came to Bury Caesar not to Praise Him. I thought about starting this talk with I’ve come to Praise SSRIs not to Bury Them. SSRIs work – it’s doctors who are not working.
The hazards you’ve heard about may leave you figuring we need to bury SSRIs. Listen up. Unless we realize how valuable a scientific and therapeutic tool SSRIs can be, Doctors risk being Buried.
Slide 39. The Federal Aviation Authority (FAA) licenses planes the way FDA licenses drugs – by looking over paperwork. FAA don’t keep you safe in the air – pilots do. They have an incentive – if you don’t get to New York, they don’t either.
Doctors are health pilots, not FDA. But if the door flies off a healthcare plane and you draw attention to this the incentives tell doctors to throw you through the opening for spreading Treatment Hesitancy.
Slide 40. This is an inevitable consequence of Doctors Delegating Narcissism to bureaucrats. Journalists researching adverse events hear doctors telling them people claiming to know they have PSSD, for instance, have Narcissistic Personality Disorders.
When growing up, we Delegate our Narcissism to father figures. Later when confused we may delegate it to dictators, or gurus. Delegating it to bureaucrats suggests extreme vulnerability. Managing Treatment Hesitancy for life-saving treatments is one thing but as Goldman Sachs have told us, making drugs that save lives is a bad business model – the pressure to push down the price of life-saving drugs is huge. Companies make cosmetic or identity disorders to sell profitable drugs, using doctors who they view as devoid of a thought in their heads not put there by them as the front of house sales force.
We are not dealing with a Big Pharma making life-saving drugs, but with Big Propaganda, whose propaganda has become invisible. Behind EBM and Follow the Science labels, and a chorus line of Narcissistic Disordered Doctors, singing Let’s Do the Narcissistic Tango Again we no longer see this.
If their defenses are challenged, as doctor’s are when someone turns up with very Evident adverse effects, narcissists get aggressive and pick on victims. This system breeds violence. Clinical psychologists seeing the same patients as doctors are mostly too scared to hint that obvious side effects are treatment related for fear of a threatening email or worse from a Medic telling they are not licensed to practice medicine. This isn’t just bad healthcare – it flies in the face of Science.
A note of caution is needed here. I am not talking about Bad People. I am talking about a Bad System. You may need to be as close to the pharmaceutical industry as I’ve been to see how the System works.
Slide 41. In The Antidepressant Era 30 years ago, I offered a thought experiment. What if these drugs were over the counter (OTC) rather than prescription only. This wasn’t a policy proposal. I was drawing attention to the fact that since 1962, to give you Prozac FDA regulations require me to give you Depression. I need to disable you. If I do this, we have to be sure we are going to bring good out of this injury.
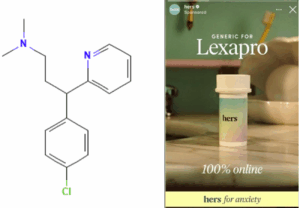
Switching to OTC bears thinking about as a policy proposal now. The molecule on the left is a potent SSRI that can cause all the problems SSRIs cause but if Woody Witczak had taken it and not Zoloft he would be alive today. Why? Because chlorpheniramine is OTC, and if it didn’t suit Woody, uninhibited by a good doctor, he’d have stopped it. Do doctors add value here?
If our drugs work as well as we are told and are as free of problems, doctors aren’t needed. Nurses and pharmacists are cheaper prescribers and maybe safer than a narcissistically challenged doctor. Doctors deserve to be and are rapidly being buried.
In The Antidepressant Era I also said that if these drugs were OTC companies would ensure all of us – not just doctors – wouldn’t have a thought in our heads not put there by them. The use of Tylenol in Pregnancy, is a great example of this.
Hims and Hers, and other platforms, now sell prescription drugs OTC – see Authenticity Inc. Telehealth and Influencers. The Creation of Psychopharmacology 25 years ago spelt out how companies like this would ambush us. They use instruments, like rating scales, blood tests or bone scanners, to create figures which their drugs can put right for us.
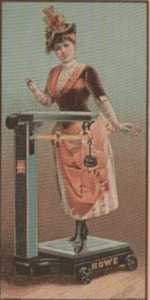
Slide 42. Checking the figures for our weight began in France in the 1860s. A decade later a new disorder was born – anorexia nervosa. Fasting had been a way to holiness, but became a health and beauty matter. Figures can hypnotize us as easily as icons or incense can.
Companies now create Food Noise scales – See Authenticity Inc – designed to show Glyp-1 agonists muting distracting food noise.
Social Media is full of Apps generating figures, Treating figures gives the appearance of science rather than the appearance of a Neurotic Disorder.
Weighing scales and rating scales hypnotizes us. Scans and blood tests hypnotize doctors.
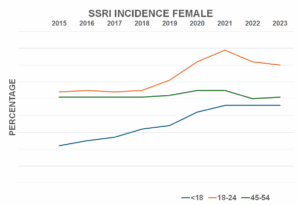
Slide 43. Here are rarely seen figures for rates of starting SSRIs among Australian women. The Green line shows figures for women in the 45-54 age bracket who are representative of all older women. The red line shows the rate for 18-24 year olds and the blue line is for 10-17 year olds. In 1990, Antidepressants were rarely prescribed other than to people of middle years but driven by social media they are rapidly becoming drugs for younger folk.
The prevalence of SSRI use for middle aged women is 4 times higher than the incidence figures – breaking up with SSRIs is hard to do – and so prevalence increases with age. The prevalence for 10-24 year olds can never catch up because unlike Peter Pan they do grow up – even so prevalence rates in this age group are rising faster than for any other age – up 110%.
These incidence figures above are for prescribed drugs. How would they look with Hims and Hers online supplies added?
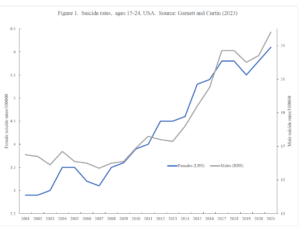
Slide 44. The gray line is for suicide rates among 15-24 year old males over the last decade. They are 4 times higher than the blue female 15-24 year old rates but both are rising at the same rate. And we now have the first legal cases for suicides after contact with Hims and Hers – Authenticity Inc Meets Grok.
Slide 45. The blue line shows the most solid finding in all of the social sciences – 600 studies showing unhappiness with life is most marked in the 40-60 age bracket and until 2018 least marked in under 24 and over 64s.
But the redline shows a dramatic shift – unhappiness is now most marked among 18-40 year olds. Are these canaries telling us this mine is about to collapse?
We now have a social welfare crisis with this generation branded Generation Sicknote and talk of countries collapsing beneath the burden of disability payments – See The Great Silence and Damsels in Distress.
Slide 46. Science began in London in 1660, when a bunch of men began holding events at which they did things like transfused the blood of a young dog into an old dog and observed – it seemed invigorated. Or looked down a microscope to see what they called microbes – were these animals?
These Events produced Observables about which the witnesses, like a jury, were challenged to come to a consensus. Science like a legal trial is an experimental process – it is not something to be followed. It is not a religion – See Health, Care and Science in the Real World.
A Case Report was made for the event and its consensus. No industry or regulators branded these as Anecdotes. This anecdotal process put men on the moon, decoded the human genome and extended life expectancies.
Medical journals came 200 years later. RCTs and their statistics 300 years later. The 1950s was the stellar decade for drug discovery when almost all classes of medicine we have now came into being. None of these breakthroughs involved RCTs. Many of these drugs, like imipramine, which people could see in real life had the capacity to work even if they also had the capacity to cause bad trips, remain better than later treatments. Life expectancies have been falling since the introduction of RCAs – especially in the United States.
There are no observables with an RCT. There are figures but figures are not observables, least of all when processed through statistical models. People are the data and especially with RCAs no person (or their ghost) entered into the study can be brought into Court to be examined and cross-examined.
You are not going to hear that this man with an improving Depression score, who dropped out of a Zoloft trial coded as nausea, was in fact Homicidal and Suicidal. Or a man, whose death was coded as burns, was so agitated he poured gasoline on himself and set fire to it intending to commit suicide.
No ‘investigators’ listed on the authorship lines of these ghostwritten (or AI generated) papers can be brought into court to testify because none of them have seen a person given this drug.
None of this is Scientific Evidence. It’s Hearsay.
In contrast, every time we prescribe a drug to someone we initiate an experiment that takes place in front of us or can do if the observers make it possible to observe what is happening – see below.
When we prescribe any medicine we open a door to the purist form of science there is and with SSRIs we have a tool with which to explore some of the most fascinating issues imaginable.
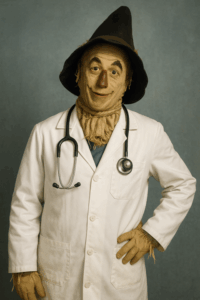
Slide 47. Before engaging in pure science, this scarecrow, as in The Wizard of Oz, needs a brain, a heart and courage, given to him by an ordinary girl, who may have dilated her pupils to fool him into thinking she thinks he’s amazing. Of course the uniform needs to be removed.
He’s supposed to be a professional. That means he puts you and what you need before Church or State, the guideline issuing folk, who want him to get you to conform to what they want you to be.
Rarely in the course of human history have such a small group of people held so much power over the lives of so many as doctors have with prescription-only meds. It’s extraordinary that we doctors find ourselves in such a weak position today.
Doing science means having people with different points of view in the room willing to observe and come to a consensus. It means recognizing the person who takes the pill has a privileged position on the observables, as do family and friends.
Becoming suicidal on an SSRI or having other strange experiences on this or other medicines poses a huge challenge to the scientific enterprise – those with a privileged position to observe what is happening will often be understandable wary of telling others much if anything about the thoughts now going through their head, Woody Witczak did not tell Kim that his thoughts included killing her.
Psychologists are important as we are talking about using drugs to shape behavior not cure a defect. Social workers and others count because context is important, and the pill-taker may need rescuing from a doctor hypnotized by figures abstracted from a bigger picture. These others are important because of their bias – not because they have no bias. You should only let yourself be treated by a doctor who is not just open to other voices but actively engages them – especially yours.
Exploring how SSRIs might help needs sophistication – that is an ability to hold contradictory or ambiguous details in mind at the same time and still function.
There are at least 3 steps to better therapeutic outcomes wins with SSRIs.
- Reducing the dose to at most a quarter of the usual dose, or less – the equivalent of 2-5 mg of fluoxetine, would give a better than the 1 in 6 Good Trips found in company trials.
- Doctors specifying what they want an SSRI to do to help a person – they cannot say they will get you well. They have to specify the step on the way to helping, just as with a beta-blocker we would say this will slow your heart rate and ease any shake in your hand or voice or with a benzo we would say this will relax your muscles.
- Recognize that what we call SSRI side effects are often the core action of the drug and not a side effect – they are adverse effects because the usual starting dose for SSRIs is at toxic levels.
- Getting the person taking the meds to interocept the sensory changes that start within an hour of the first dose. This may enable him/her to titrate what is happening to the right level for them or stop a treatment if need be.
Up the 1980s medicine centered on the problems people brought us. By 1990 we were bringing people into our clinics to screen them for risk factors etc and essentially were giving them problems they didn’t know they had and often adding in treatments they didn’t need.
When a person brings an ‘adverse event’ to us – this is traditional medicine. They are bringing us real problem and need traditional medical wisdom and relationships.
Beyond therapy, the boundaries of science need pushing forward. Good Science is not a matter of knowing research methods and applying for big money grants. For a doctor doing science can pay for itself – you get to trade 100 heartsink patients for 100 free research assistants whose skin in the game is a better qualification for meaningful input than university qualifications.
For psychiatrists who want to remain in the one true faith, this approach offers the chance to follow in the footsteps of Emil Kraepelin no less who with Wilhelm Wundt in the 1880s created Pharmacopsychology. Using caffeine, alcohol, cocaine and opioids then, it seemed obvious to Kraepelin and Wundt we had new tools to investigate who we are.
Kraepelin would have died for access to an SSRI. Our subjectivity, no less, is up for exploration and SSRIs on one side and LSD on the other offer wonderful tools to explore it.
But instead for the last 150 years this science has been ignored. Never in the history of science have so many observations by so many people been jettisoned by so few – and things are getting worse.
One reason why the sensory impacts of SSRIs have been ignored is that the science of the sensory nervous system has been seen as too subjective – especially by neurologists, who like the reliability of tests for the peripheral motor system and increasingly brain scans, but steer clear of a system whose responses can change from moment to moment and with both time of day and time of the month, and can vary hugely by personality type and emotional state. The only tests in common use for the sensory nervous system are biopsies to count the number of nerve endings in skin and even these correlate poorly with what people report.
Catatonia is among the most fascinating subjective mysteries. It lies on the boundary between voluntary and involuntary actions, between assigning responsibility or deciding it doesn’t apply. LSD can trigger catatonia. SSRIs can relieve it.
Hypnosis is another state. SSRIs facilitate it. What does that tell us?
Toxic doses of SSRIs can leave sexual. balance and visual problems in their wake. A genetic variation in PIEZO2 proteins causes sexual, balance and vision problems. PIEZO proteins (1 and 2) are sensory receptors whose existence we stumbled on just over 10 years ago. What other elements of our sensory system are out there waiting to be found? Humility rather than arrogance should be our default mode.
Before SSRIs and Viagra, male impotence or premature ejaculation were viewed as anxiety based neuroses needing months or years of damaging therapy dissecting personalities and histories. Lidocaine gel made penises less reactive before SSRIs – what does lidocaine say about the degree of brain involvement in Serenic effects?
How many other states might be helped by a judicious use of drugs to shape behavior rather than correct a disease?
Women disabled by dyspareunia face all kinds of protracted therapies aimed at rooting out their problems. Changing partners can solve dyspareunia (and premature ejaculation). We get told that’s because the new partner is more sensitive. Do we know for sure that’s the case?
In a group of couples, try asking how many women think they could only marry a man with the right smell? Chances are half the women will instantly endorse the idea with others looking flummoxed. What happens when your partner tells you your smell has changed since you began that drug? What happens if she develops parosmia on an SSRI – that might endure for years after stopping?
How much do we know about Material Me or about Material Us?
As Mark Anthony might have said:
The evil that wonder drugs do lives on after them –
the good is oft interred with their bones
These earlier posts touch on similar themes:
- Who’s Afraid of Science
- Healthcare Gone Mad
- Probity Blockers and Trans Medicine
- Health Care and Science in Real Life
- Die RxISKing it
- Die RxISKing it 2
The notion of Interoception comes up in the talk. The posts below deal with this in more detail.
Pharmacopsychology – forthcoming













“Unless we realize how valuable a scientific and therapeutic tool SSRIs can be, Doctors risk being Buried.”
I gotta admit, I’m puzzled by this statement. You’ve said many times that SSRI’s are useless in severe depression. You’ve also demonstrated that as an anxiety treatment they are more hazardous, not less, than benzodiazepines or other remedies. And you’ve made it clear that the emotional distress they are marketed to relieve is usually not crisis-level and is often situational and time-limited.
And even if the pills “succeed” in relieving anxiety and distress around job, school or relationship problems, they can still have profound long-term effects. Those can include emotional blunting, profound sexual dysfunction and other physical and even cognitive problems. They can take a huge toll if continued long-term and wreak utter havoc if discontinued. (It’s possible your friend Dr. Roberts could have come to appreciate his “mellower” less high-strung personality on Zoloft, and decided to stay on it long-term. Where would he have found himself ten years later?)
Finally: so far, no one can tell us what duration of use is “safe” or “smart,” or who will or won’t suffer permanent effects. So no, we cannot “just try” an SSRI, secure in the knowledge that if it “doesn’t suit us” we can just stop with no harm done. It appears to be a total crapshoot.
To say nothing of the fact that so few of the people plunged into profound agitation can make any kind of spontaneous link between the pill and their emotional state. They don’t go back to their doctor pleading to stop the pills – they go back completely clueless as to what is happening. If their doctor tells them the pills “do nothing” for the first 4-6 weeks, as Woody’s doctor did, they readily believe it. Some even continue the pills when told to stop.
I am no big fan of alcohol or benzos—I know first-hand how addicting both can be. But I find myself thinking that if Woody Witczak needed any chemical treatment at all for his short-term “nerves,” a tab of Xanax or a shot of whiskey at night would probably have been more effective. And definitely much, much safer.
Maybe there is a condition out there for which SSRI’s are a terrific therapeutic tool that we mustn’t even think of giving up. But what exactly is it?
Jo
When patients can spot a doctor doing well on an SSRI – can spot a real change in him consistent with what the drugs do – and the same doctor later says yes, he can see how this might help him if he had a nervous problem, then it is clear SSRIs can do something that could be useful.
When psychotherapists not usually known to be in favor of meds can see an SSRI effect very clearly and can see it might or might not be useful depending on the circumstances then clearly these meds can be useful. Likely useful in no more than 50% of folk at best but still useful – and a very different effect to benzos or beta-blockers so having another approach is also useful.
The problem and the burial issue is what at doctors adding to this. Woody’s doctor should never have given him an SSRI for poor sleep but most people including doctors see SSRIs as a coping tool – something to help you grapple with stress.
The difficulty is good doctors give these things because they are labelled as working without saying what we want is for it to do X which may or may not suit you. Instead they are dishing out magic – it is just going to work.
They do the same with antihypertensives and hypoglycemics and almost all drugs – they should be working out what kind of antihypertensive or hypoglycemic I need and giving me that – instead I risk ending up on 4 different antihypertensives or hypoglycemics and at increasing risk of dying prematurely from my meds rather than from any underlying condition
So tell me what value are doctors offering in this situation and if none – if they are increasing the risks – when do we think about changing the system and what is it about the current system we do not want to replicate in any replacement?
Finally the ultimate lunacy in Woody’s case was telling him to hang on in there for 6 weeks. There is no basis in anything for this idea
It would be nice to have something to Praise doctors for. Difficult to blame FDA. They figured we just license these things – we expect doctors to be sensible when it comes to using and to work out how to use them.
D
I wish I had known, David and André Marx.
I’m sure I could’ve worn a tie and made an audiance appearance.
If people would’ve known how bad the state of pharmaceutical ‘Sciense™’ is, I could’ve made a contribution too.
But I simply cannot raise my voice as long as nothing as much as ripples the surface, despite the years and efforts of ‘psych-meds-movement’.
There has been serious concern about brain pills for 70 years or more, but nothing changes.
Now they say that we ‘could’ be hurting kids with a crowded vaccine schedule, and what is allready established is that proper and rigorous testing for vaccine safety against proper placebo, is just not there.
Yet, attending such an event would be a bliss, because in my fantasy, I do try to help.
Ove
It’s the no ripple problem. How do we create a ripple? That’s partly what this lecture is trying to grapple with – by the back door. Ranting about hazards and warnings does nothing, maybe even makes things worse. What about saying we could be doing so much better? Only 1 in 6 folk have a good SSRI trip now – can we get this up to 1 in 5 ? And if doctors can’t do this – what can they do?
D
There was a comment from a colleague at one of the lectures that he had been giving SSRIs at double or triple the Prozac 20 mg dose and had never seen anyone become suicidal.
There is a reason doctors don’t see the problem. One of my very first patients who became suicidal told me nothing until I had the idea of giving him a benzodiazepine to get him to relax and then the story tumbled out.
But the most compelling illustration of the problem came with one of our healthy volunteers – a woman we all got on with very well whom no-one spotted was suffering badly, It was only after the study was over and she survived that she confided that if anyone knew the thoughts going through her head she figured that we would have locked her up. She, like many people even doctors, do not necessarily or at least quickly make the link to the medicine they are on.. You might go into a sensory deprivation tank thinking you know what to expect but when ambushed by the tank it looks like we can all lost the plot
D.
Another comment from a different colleague was that the psychiatrists tell us that we are using too low doses – that we have to go up to Prozac 40, 60 or 80 mg.
The problem going up to higher doses is no one then knows what they are doing. Anything beyond Prozac 10 mg is stepping into terrain where the drug is doing something other than acting on serotonin and no-one knows what. It’s flying blind rather than being in control of the aircraft.
D
Sensory Impairment’
the core action of SSRIs are their sensory effects.
One has the impression everything has been wiped out and there is no mind anymore.
Rarely in the course of human history have such a small group of people held so much power over the lives of so many as doctors have with prescription-only meds. It’s extraordinary that we doctors find ourselves in such a weak position today.
‘Precautionary action’
https://www.bbc.co.uk/news/articles/c8e9d13x2z7o
Around 6,000 Airbus A320 series aircraft were grounded for urgent software modifications after one suddenly descended rapidly, injuring several passengers. It seems that updated software was flawed and the previous version is now being re-used.
This shows that all modifications need thorough testing before use but errors can still slip though. Luckily the aircraft industry puts safety as the first priority.
Doctors are still experimenting on patients, with millions reporting injury and death, and the medical profession are ‘flying by the seat of their pants’.
Shouldn’t Doctors have the same regard for life as Aviation.
Annie
Important comment – except in this case it is the Company taking actions that pharmaceutical companies also used to take before Lilly and SSRIs – they introduced warnings and decent information aimed at making taking a drug safer. But the information now in place makes the drugs more hazardous than they should be.
Doctors are missing in action. It’s a bit like you’re on a plane and you see the pilot jump out opening his parachute on the way leaving you to wonder what’s going to happen.
David
Gosh, there’s so much to take in here. One point which I read here,
and have heard you mention before, is around the use of lower doses
when first given a prescription for psychotropic drugs. Is this
something we should be encouraging pharmacists, for example, to take
on board and then, maybe, share such with doctors? In your opinion,
are doctors likely to listen to pharmacists? Do we, as patients, have
the right to push for a lower dose if we were in such a position as to
be offered a prescription? One major problem, of course, is the lack
of low doses – what the companies call ‘low’ is obviously too high for
many isn’t it?
Now, to those trapped on doses which are causing them severe problems.
To me, it makes sense to reduce by very small amounts – the smaller
the reduction the smaller the reaction – is that so? If so, then
shouldn’t we be pushing the companies for the production of lower
doses rather than expecting patients to be counting beads or shaving
bits off a tablet? Production of liquid formulation at much lower
costs would surely be helpful in such circumstances.
Finally, from where has come the idea that more is always better in
the prescribing of psychotropic drugs? Is no notice ever going to be
taken of the lives ruined by sticking to an idea that if you drug
someone to the hilts then that is better for the patient?
Mary
It is one of those things where what looked like a clever move to some company dudes nearly 40 years ago has resulted in chaos now with no-one prepared to or left around to own up to a mistake. Lilly did the 5 mg trial 40 years ago but the report of this study costs you money to download.
You are not going to get pharmacists to do anything much to help you unless they are a compounding pharmacy. You can insist on liquids but family physicians will be slow to offer this as it costs them money.
Re tapering. In principle this makes sense if the only problem the person has is a physiological dependence on the SSRI. It does not make sense in the case of PSSD, PPPD, VSS – and other problems – where there has been damage. If you have been damaged, the worry is that the longer you stay on the medicine the more damage there is likely to be.
Nightmare on Pharma Street? And worse again there are no doctors able or willing to tackle the Freddy Krueger going around killing us all
David
Doctors constantly sit-tight in their ‘feeling’safe-zone. They are a protected species. They are protected by the Guidelines from NICE, from the MHRA, from the UK Royal Colleges of Psychiatry and GPs, from Louis Appleby, Simon Wessely, Wendy Burn and even from those who promote hyperbolic tapering.
The US American Psychiatric Association.
The US Secretary of State is looking in to associations between violence and homicide from SSRIs.
David’s comments above about Doctors raising the prescribing is shocking and terrifying. Also the fact that sometimes it is like getting blood out of a stone for patients to describe what is going on ‘in their heads’ when patients are not able to realise that it is what’s going on in their bodies that their brain cannot compute.
If doctors don’t and won’t understand this, then the hazards will run amok.
A huge stab, cutting through the odds of a doctor understanding something when his whole career is based on his not understanding it. The SSRIs created a doctoring monster entranced in magic – this is the impossibility of the situation. As one of David’s anecdotes said, if she admitted to her thoughts, she could be locked up. This is more than an innocent fear.
I wish we had monster doctors. We have badly shrunk shrinks – along with other shrunken doctors. I have heard company people telling doctors we figure you don’t have a thought in your heads not put there by us – and it makes no difference to 99% of docs. They must think it’s a friendly tease.
D
‘SSRIs work – it’s doctors who are not working.’
If this, as I see it, is the sharp end of your counter intuitive strategy, then I think it’s a necessarily provocative move. Particularly coming from you.
Ranting is entirely appropriate given the scale and intensity of harms, but the system is inured to it, as you say.. Although it is the bedrock of what comes next. 30+ years of ranting to move the needle on SSRI safety comms. I know you’ve seen the press release – ofc no judgment until we review the actual material- but for anyone who hasn’t:
https://www.gov.uk/government/news/patient-and-family-experiences-inform-antidepressant-safety-information-review
You asked a fundamental question- ‘why can’t they spot effects? ‘– and answered it here and elsewhere. It’s perverse how little prescribers actually understand about SSRIs. It’s all completely EXTRINSIC – i.e. ‘not part of the essential nature of something’ – Industry mythology and fragmented guidance based on it, with not a whole human being nor a therapeutic principle in sight.
This is STILL how fluoxetine is described in its current PIL- shameless marketing garbage:
‘Everyone has a substance called serotonin in their brain. People who are depressed or have obsessive-compulsive disorder or bulimia nervosa have lower levels of serotonin than others. It is not fully understood how Fluoxetine capsules and other SSRIs work but they may help by increasing the level of serotonin in the brain. Treating these conditions is important to help you get better. if it’s not treated, your condition may not go away and may become more serious and more difficult to treat. You may need to be treated for a few weeks or months to ensure that you are free from Symptoms’.
And the NICE guidance for e.g ‘ more severe depression’ is mostly such a laundry list it verges on satire in places. The reference to ‘medication effects’ is novel – but they don’t spell out what they mean nor why:
‘SSRIs are generally well tolerated, have a good safety profile and should be considered as the first choice for most people.
Usually taken for at least 6 months (and for some time after symptoms remit).
Choice of treatment will depend on preference for specific medication effects such as sedation, concomitant illnesses or medications, suicide risk and previous history of response to antidepressant medicines’.
The therapy options read like the menu of a rather pretensious restaurant:
Guided self-help, Interpersonal psychotherapy, short term psychodynamic psychotherapy, counselling, individual problem solving, individual behavioural activation, individual CBT.
https://www.nice.org.uk/guidance/ng222/chapter/Recommendations#treatment-for-a-new-episode-of-more-severe-depression Whatever happened tio just – listening and being present.
And given what we’ve learned from you about dosage levels and rogue small molecules, recommended doses seem dangerous. For example:
Fluoxetine : Usual minimum effective dose 20mg, maximum 60mg
https://cks.nice.org.uk/topics/depression/prescribing-information/antidepressant-dosing-titration/
It is absolutely right that the focus has finally landed on deprescribing – tapering at the patient’s pace, mostly slowly and carefully. . But ironically, all the receptor occupancy malarkey places the action back in our brains again, not our sensory systems.
I know huge numbers of people in the prescribed harm community. But also some for whom SSRIs have been so useful any adverse effects were far outweighed.. Middle aged women – as usual – going through situational unhappiness and stress – a grisly divorce, elderly parents ill or dying during Covid restrictions etc. They said they were given low dose SSRIs (low dose – who knows?), short term – specifically to ‘take the edge off ‘ the difficult situations they were navigating . Translating this into sensory system MOA thinking – they were DESENSITISED..
I find it difficult to do anything other than laugh derisively at the MHRA and their EWG press release – the biblical reference to Straining at Gnats and Swallowing Camels comes to mind
How any self-respecting doctor or anyone who has been harmed by these meds could give MHRA any credibility is beyond belief. It used to be said if all the medicines we have were sunk to the bottom of the sea, it would be all the better for us but worse for the fishes. If the MHRA were sunk to the bottom of the sea – and any doctors who pay heed to them – we’d be a lot better off
D
The Lost Leader
He didn’t come, and he buried them
Examination of Witnesses, minus one
Ex GSK, Head of MRHA, Ian Hudson, could have helped things along, but, of course, he wasn’t allowed anywhere near Paroxetine meetings, as a Government Official discovered at a Seroxat inquiry, when he enquired ‘Where was Ian Hudson?’
It’s hard to believe, after the flimsy excuses as to his non-attendance, that the Government Official let this go, but he gave a clear indication of what he thought about it.
https://publications.parliament.uk/pa/cm200405/cmselect/cmhealth/42/5012003.htm
Q790 John Austin: I think it would have been useful if Dr Hudson had been here because, as far as I understand, he was at SmithKline Beecham and his department was responsible for the collection of adverse reaction information such as there was with Seroxat.
Q791 John Austin: So he would have been a very key witness.
The biggest joke, since ‘like rats in a sack’
For readers not familiar with Ian Hudson – he had been the Chief Safety Officer for GlaxoSmithKline and claimed in the Tobin trial GSK has no evidence that Paroxetine could cause suicide – when it had abundant evidence this was the case. He left GSK and had joined MHRA when the Suicide of Children on paroxetine crisis blew up and as these marvelous quotes reveal he was hidden away when the scandal was being investigated.
A few years later he become boss of the MHRA – Britain’s equivalent to FDA. It’s just one of the many reasons never to Delegate Narcissism to bureaucrats.
D
In your position, having exposed the risks of SSRIs for decades, I’m not sure I’d even be able to muster derision. I’m curious to see the MHRA Expert Working Group produce that has taken 30 years along with 18 months of experts meeting to write.
Marion shared an editorial written a long time ago that you will know well – written by Wessely and Kerwin in reaction to the seismic effects of the Panorama series – 20 + years ago stating:
‘The results confirm that antidepressant prescription is indeed associated with suicidal behaviour, and strongly so. This simply means that antidepressants are being prescribed for the right indication, and that they do not immediately eliminate suicide risk. That we knew. The article by Jick et al also shows a 4-fold increased risk for suicidal behaviour for patients first prescribed an antidepressant drug within 1 to 9 days before their index date. This too is not unexpected—patients see their general practitioner when their distress is most intense.’
But the hypothesis being tested is that over and above the known association of antidepressant prescribing and suicidal behaviour (in which the confounder is the presence of depressive disorder), there is also a specific link in which one class of antidepressants, the SSRIs, increases that risk still further. The results do not offer much support for the hypothesis. ‘
As much as the content, the faux airy tone with which the risks to human life are seemingly dismissed by authors, Wessely and Kerwin, says it all. They know the risks are real, we know they know the risks are real, but closed shop religions are so good at circular reasoning and self-justification, they almost persuade themselves. They go ‘full firehose’.
There are rather a lot of provocative strands and levels of thought in your talk. This one in particular has resonated on X – amongst patients and peer support:
‘The problem going up to higher doses is no one knows what they are doing. Anything beyond Prozac 10 mg is stepping into terrain where the drug is doing something other than acting on serotonin and no-one knows what’.
As one person commented– ‘Honestly, dosing feels more roulette than science past 10mg.’ And they’re right.
Obviously much of the focus of patient safety campaigning in recent years has been on tapering and deprescribing – quite rightly – given the millions on SSRIs. But, arguably, many more lives would be saved in the future – and conceivably more patients might even benefit from SSRIs – if they were being prescribed at effective rather than toxic dosage levels. I know Tim has said this in the past- this really needs to be a big story.
David
I have taken some time to think about what you are conveying – and it does make for mind-blowing reading.
As I understand it you are saying the PRIMARY actions of these SSRIs are on the sensory systems (peripheral nervous system, PNS) of the entire body/essential physiology.
The effects of the drugs are then relayed back to the primary spinal cord control area as likely needing corrective attention which homeostasis then attempts to deal with – resulting various knock-on effects on physiological and psychological functioning.
This primary PNS action of these drugs has been completely overlooked – so SSRIs that we have been using liberally for decades to treat ‘mental health’ issues have resulted in all manner of physiological and psychological problems. The ‘side-effects’ are the primary effects!
Have I understood this correctly?
The BMJ has published a response which I submitted on 30 November:
https://www.bmj.com/content/346/bmj.f191/rr-1
Marion
Yes the primary effect is on the sensory half of the peripheral nervous systems. Yes, many of the effects are not side effects, they are part of the core effect. They are adverse effects but not side effects – adverse because the doses most people start on are toxic to begin with and the core, sought-for effect, is unmanageable as a result
David
When the Adverse Effects kick in, everyone thinks it is the brain making decisions. As David explains it is the bodily senses that are driving this.
In all the adult cases we have read about, Woody Witczak, Stewart Dolin, Donald Schell, and recent children, Romain, in France and Dexter, in Canada, you have to ask yourself. Did they seriously decide to use rope, trains and guns to end their life. These are all intelligent people, whose brain of thinking, did not advise them to end their life in these dramatic and horrific ways.
The sensory overload was so huge, so all encompassing, that it could not be stopped.
In every case, where we rely on our brain to give us directions, this was overtaken. You don’t wake up one day and make a pragmatic decision, that today you are going to blast your family with a shotgun, throw yourself in front of a train or hang yourself with rope.
In every case, it was a split-second, monumental misfire, which the brain could not adjust to. The brain was so sabotaged by spontaneous eruption from all the attacks from the body, that the brain shut down from the thrust of it, so all the normal thinking these people had for their entire lives, disappeared in an instant.
We rely on our brain to keep us safe. Doctors tap our knees to test our reflexes and if our reflexes are fine, our knee will jump. This is our body communicating with our brain.
When the sensory overload hits a peak, the brain is rendered an adjunct of complete paralysis.
The frozen moment, when time stands still, the frozen moment, when rational thought goes out of the window, the frozen moment, when bodily impulse evades all common sense.
It is a hard principle to swallow, but you only have to look, to see, to experience, the way this works.
People who have not experienced the hard shift from reality to death, or almost death, will find this a very difficult concept to accept.
Because, they have never experienced a ‘brain-stoppage’ and never will, and this is why the ‘core of sensory’ escapes them, and they don’t understand it.
Thank you..
This makes a lot of sense!
Thanks for your comitment and perseverance in this field David!
Hamed,
General practitioner, Sweden
Hi again,
Forgot my questions:
1-I wonder why you choose 5mg as a good dose for Prozac? According to the diagram it is equivalent to 60% receptor-binding.
2-How variable is this receptor-binding in different individuals? can someone get 5% and another one get 90%?
Regards,
Hamed, GP
Hamed
Great question. Generally speaking 80-85% binding has been viewed as full de facto receptor occupancy – you don’t get more benefit going above this and you increase the risks of breaking the system. A key point is that we also don’t know what else these drugs are acting on even at 5 or 10 mg. We have to accept that it’s likely that above 10 or 20 mg these drugs are increasingly likely to be acting on other likely important systems such as carbonic anhydrase. Companies may well know the answer to this but aren’t telling us.
You’ll notice that at 10 mg receptor occupancy is coming pretty close to the 80% point. There is not much point going higher. Why 5 mg – well a key point is that identifying a muting of sensory reactivity as what the meds are working on gat 5mg this gives the patient a better chance to identify the effect we are seeking and work out whether this is likely to be something that helps him or her or not.
You are absolutely right there can be variation between people. It looks like some people get a different functional effect from SSRIs to me and perhaps you – they don’t have sensory muting at all. Their genitals for instance do not go numb. In cases like this we have no idea what is happening on the reuptake site – they may have normal binding but just not the usual functional effect
Companies really interested in patient care and in science should have been encouraging us from the start to keep an eye out for things like this and supporting us to explore these effects. This would have created a climate of confidence among patients and doctors as to what we are doing instead of the bitter wars between patients and between clinical colleagues that we have now.
But billions of dollars profit and several decades later we are now wiser – indeed clinical practice has been dumbed down. Some of these issues will be dealt with on Monday in two new posts Pharmacopsychology here and Treating Narcissism on RxISK.
David
Forgive me, I’m meant to be completing a stats assignment and my psychiatry textbooks are under a pile of rubbish and takeaway containers. Can you remind me why melancholia is considered a disease of mid life? Do you mean that you equate melancholia with involutional melancholia? And in turn, do I take it that you equate it with vital depression? So what are the younger cases?
This could be a longer answer than the original post. Forget your books – almost none of them will now hint at what happened. You have to have been there to have some sense of it
First melancholia in middle years was very distinctive through to the 1980s. Almost as distinctive as catatonia. Impossible to view as what gets called depression now. It rarely brought people to see a doctor prior to tricyclics. It could get so bad you were hospitalized – especially if you developed delusions – and when ECT came along you got ECT. It and Catatonia were the two conditions that responded to ECT. Melancholia responded to TCAs catatonia didn’t. The pictures though could be confusing – it was easy to diagnose someone as having melancholia when they may have had catatonia but were still at a mobile stage.
Endogenous depression or vital depression overlapped heavily with this. SSRIs were relatively useless for all 3 states. Many people clearly got endogenous or vital depression – melancholia – and didn’t seek help. It might take weeks or months but they recovered naturally. Even the most severe hospitalized cases recovered naturally without treatment in 5 months or so on average.
Could young people get – yes. It’s just they didn’t present. The typical presentation as the drug company adverts in the lecture show you was in middle years. Some shrinks, including Kraepelin, at one point bought into the idea that this was an involutional illness but that vanished.
Among the untalked about factors that led to a change was the Dexamethasone Suppression Test. This test of cortisol levels distinguished endogenous depression from neurotic or reactive depression. DST positive folk responded to ECT and TCAs but not to SSRIs. Neurotic or reactive depressions were not DST positive. With the advent of the SSRIs, the DST and melancholia got written out of the script.
You’ll find it hard to find a book that lays this out for you. The idea that DSM was following the science looks pretty weak in the light of this. DSM has an opportunity to build DST tests into their criteria for what they called Major Depressive Disorder – which sounds vaguely like Melancholia but is a world apart from melancholia.
A key point to keep in mind though is this. Lots of people with melancholia clearly used to live with it and almost certainly did pretty well handling it that way – maybe even better for them than if they had sought medical input.
We hear a lot these days about overdiagnosis and shrinks are wheeled out to say – hold on the problem is underdiagnosis. And a case can be made for this. You could do a community survey for people who meet criteria for melancholia who aren’t in treatment and leap up and down claiming we need to detect and treat these people. Quite aside from the fact that giving them an ineffective SSRI would be a disaster, lots of us who opt not to engage with the medical system from various things are quite possible doing exactly the right thing – but the system and lot of doctors can’t bear this idea.
It’s almost like the system currently being unable to leave teenagers untreated. Adolescence is being heavily medicalized – which will have the added benefit for companies of generally lowering the barrier to medical system engagement for the rest of your life.
Having hopefully driven a stake through the heart of under-diagnosis, it’s time to say Under-Diagnosis is Dead, Long Live Under-Diagnosis. Doctors and Medically Systems are chronically and disastrously under-diagnosing the very real disorders their drugs are causing
D
Thanks for the detailed response. I really do appreciate it. I sometimes think you would have made a fabulous nosologist if Pfizer hadn’t so utterly commandeered your time explaining the tediously obvious. I really don’t know how you manage to keep such patience as a full-time Woozle debunker and know I don’t help with my constant requests to identify yet another this or that Woozle.
That actually is a pretty good match for what I’ve read. The books currently buried are M. A. Taylor’s Neuropsych textbook and G. Parker’s monograph on melancholia. I have digital copies of Fink’s books and Shorter’s, as you know. I’ve also got that awful book Donald Klein wrote where he evidently had some fit of nobility and decided to forgo his own ideas in favour of humbug for the laity. I also data-scraped Barnie’s Twitter feed; it would make a lovely coffee table book – one half Trump, and then you flip it over and read him railing against psychopharma.
MTA makes the point in his textbook that true melancholics “rarely complain of depression”. Does that sound about right to you?
But I want to clarify a couple of points. Is there or isn’t there anything at all to “involutional melancholia”? I say this because one of the most stable phenotypes I’ve come across so far in my new job, and H had a couple of clients like it too, are people in their 60s who suddenly come in with wringing hands and furrowed brows, complaining that their “bowels are blocked” and that they “will most definitely die if they are not unblocked”. They come in every 12–18 months or so for ECT and seem to be right as rain afterwards. H had a client she knew well, and her husband was adamant the first attack was recent. Ditto for the families I’ve spoken to. Actually, we also get paraphrenia cases, slightly younger, say mid-50s, no prior history, suddenly convinced the neighbours are gassing the house. Now, I’m jumping around a bit bringing paraphrenia into it, but the whole mid-life thing seems to have something striking about it.
So are you saying melancholia, in your view, has nothing biologically to do with mid-life, but rather that the typical clinical presentation used to be mid-life because that’s simply when people happened to come to the attention of doctors?
Also, since you brought up the DST, I have a question that I know you know I’ve been itching to ask, so we might as well get it over and done with: what is up with the table that does the rounds showing bipolar mixed states at the top of the DST non-suppression list? I know the thresholds are more striking for psychotic depression, so I’m guessing you’re going to say that the population of psychotic depression gives a more homogeneous sample of true melancholia than the broader melancholia population, which is more likely to include misdiagnosis. I have a vague recollection from Fink and Shorter’s book that our best mate Charlie N got a thumping non-suppression result from a young man in a mixed state. Did Carroll ever comment on mixed state nonsuppression or was it Nemeroff?
Also, do you think the DST is clinically useful? Or useful in research? Given all the silly tests ordered at the hospital, I can’t see the harm, even if the only clinical utility is that it gets the young doctors thinking harder about psychopathology/physiology.
Age may color a melancholia but there is nothing to suggest melancholia is restricted to youngsters of the age of 60.
Mixeditis, mixedopathy, mixedophrenia? American shrinks discovered mixed states just before the SSRI and suicide issue blew up, and those who did became zealots. It happens with words that can mean everything to everyone. Would you, as many US brethren did, say when a healthy volunteer becomes suicidal on an SSRI that this is in fact revealing that he has an underlying mixed state rather than the drug is causing the suicidality? A Mixed state is a more comfortable idea.
Just as it is more comfortable to figure psychotropic drugs cause neurogenesis rather than neurodegeneration
D
I certainly wouldn’t conclude a healthy person was having a mixed episode if they reacted badly to a drug, that would be ridiculous. I have a natural predilection to your way of thinking, not to mention that you know what you are talking about. It does seem rather an oddly specific thing for these Americans to pick. Of all the things for them to land on, why do you think they picked mixed states?
So if those older people with the blocked bowels and excellent ECT response have melancholia, then I think you’ve just made me realise what melancholia is, and it’s not at all the same as what I had in mind.
So what are these allegedly “mixed” DST super-non-suppressors in your view? Agitated melancholia?
All I can tell you is if your super non suppressors had anything to do with Nemeroff, Barney Carroll, the creator of the DST, an Australian, Melbournian, would have dismissed it out of hand
D
Thanks for the insight. I thought you might say that about Carroll and Nemeroff. I must admit, I had hoped you would say something else, as me not being there or knowing these people puts me at a disadvantage. I hate hassling you about this because I figure you were there for some of it and so me questioning you feels obnoxious but I just want to make sure I’ve got it all straight.
I thought the fall out between Carroll and Nemeroff was over RU-486? Before Charlie started helping himself to the collection plate, wasn’t he one of the few people who stood behind Carroll on the DST? Did they disagree about the DST and mixed states back in the 80s?
You know, Nassir shared with me some of his correspondence with Carroll, and Carroll specificially included “mixed bipolar disorder” in his “A-list” of psychiatric diseases that you “know it when you see it”.
Actually, now that I reread Carroll’s email, I see that he seperates “mania, melancholia, mixed bipolar disorder”, what do you make of that?
I can see I need to reread his all of Carroll’s work. Any tips on where to look for his views on mixed states?
Actually, I just found this passage:
“Kraepelin never used the term bipolar disorder, and for good reason. The usage “bipolar,” which originated with Leonhard (12), implies closure on a question that is still unresolved, namely, the relationship between mania and depression. In one view these conditions are polar opposites: the term “bipolar” would then be appropriate. An alternative proposal, the so-called continuum theory, regards mania as a more severe form of affective disorder than depression (13). The third possibility, that Kraepelin endorsed, is that mania and depression are simply different conditions that often alternate and that are closely related to each other. This view is recommended by Sims (14). A cogent clinical reason for this position is the common occurrence of mixed states in which some features of each disorder are present simultaneously. Thus, despite the adoption of the term “bipolar” in DSM III, the original name manic-depressive may be preferable: it denotes the association of the two conditions without suggesting a formal relationship of opposites between them”. Carroll & Barrett, 1991, p. 267
Do you know if this passage represented Carroll’s thoughts? Most of that passage jibes with the things you’ve told me, in fact, whenever I find things like this I’m always struck by how faithful you are to sources. The only thing is the bit where it says “common occurrence of mixed states” which seems to imply that mixed states are at least to be bought in from the cold. I mean, melancholia, mania and mixed states may be separate things, as this passage suggests, but it seems to also imply a relationship to all three.
I’ve torn in two minds about posting this – its long, tangential to most real world interests, has too much the flavour of a private conversation and risks distracting from the points in the original post.
Re mixed states – some people with Parkinson’s disease are well known tp have on-off phenomena. Should we regard these as mixed states or just Parkinson’s disease refracted through the lens of biological variability?
Similarly people with tuberculosis can look very different if their illness involves a gut infection as opposed to a respiratory infection. If there are cases that involve both gut and lung infections should we view these as mixed states that are essentially different illnesses to lung TB and gut TB or view them as TB refracted through the lens of biological variability.
Some women get hypersexual pre-menstrually, some as sexual contact averse and some notice no change. Are two of these states different illnesses? Is one of them a mixed state? Or is it just biological variability in action?
Kraepelin very clearly said that the postpartum psychoses – that would often be termed mixed states today – were a completely different illness to manic-depressive psychosis. But for Kraepelin post-partum psychoses were nothing like what today would be called a mixed state – they had almost no features in common with manic-depressive psychosis.
As for Nemeroff, there is an interview with Barney Carroll on The Psychopharmacologists reference section linked to Shipwreck of the Singular on Samizdat Health. The views in this stand in marked contrast to what you’ve mentioned above
D