This post was written 5 years ago. It is a sequel to a lecture posted last week on RxISK with its comments – Are Healthcare and Science Compatible? The comments brought out how we now have a system that gaslights both patients and doctors leading to tensions on all sides as this post illustrates.
It also links to RxISK’s – Guilty Until Proven Innocent – Prime Facie – this week.
Reducing Medication Burdens
Between February 2020 and 2021, I was one of four psychiatrists taking mental health referrals from 80 primary care physicians in an Ontario University city.
The most common referrals were people who were anxious or depressed, who had been on antidepressants for a decade or more. Some had started in their teens. For some the original drug had cascaded into cocktails.
Another group wondered if they had ADHD or Autistic Spectrum Disorder (ASD). This group included a number of people who could be described as extraverted or introverted in temperament rather than ill. Extraverts complain of lack of focus; introverts complain about too much focus. Extraverts take risks and are impulsive, introverts manage risks and ruminate. Extraverts find the features of ADHD described in the lay media fit them perfectly. Many university students engineer ADHD or ASD diagnoses, believing the diagnoses or treatments can be used to good advantage.
Extraversion and introversion are biologically based elements that shape personalities. Medication can help but is not a cure and the treatment of ADHD by stimulants has been linked to an earlier onset of Parkinson’s disease.
A third group were under work stress linked to the management culture in factory, university and healthcare settings. These referrals asked if the person is depressed or anxious – conditions that locate the problem in the person. A neutral diagnosis is burnout or adjustment disorder, which tread the line between securing a disability payment and not locating the problem within the individual. Sometimes the management dysfunction was so clear, it had to be the diagnosis.
Few referrals had prior admissions for mental illness, even though some had up to six diagnoses and were taking nine psychotropic drugs in addition to other medication.
Mild to Moderate ‘Mental Illness’
The superficial dynamic in referrals from primary care physicians is that these referrals are for minor mental illness and a serious mental illness expert will find these cases easy. Primary care problems are not in general continuous with traditional mental illnesses.
Severe mental illnesses are relatively easy to diagnose, and the treatment options are more straightforward than many primary care cases. Primary care throws up a lot of anxiety and distress stemming from existential, or social issues, as well as conditions where the appropriate response is diagnostic and therapeutic uncertainty.
Aside from a small number of cases that may evolve into mental illness in need of secondary care or have neuropsychiatric features that specialist input can help with or may require a turn to off-label therapeutic options, primary care physicians will usually know the person, their family and circumstances, better than a psychiatrist could on the basis of a single meeting and without contact with family members or the ability to see changes over time.
There is, however, pressure on family doctors to do what specialists recommend. The image here is of a Judas Goat – whom companies use to get family doctors onside. See Partialists and Generalists.
SSRI Burnout
Some of the main treatments for primary care nervous problems, like the selective serotonin reuptake inhibitors (SSRIs), are now 30 years old. While their use has largely been proper, and helpful, professional bodies like Britain’s Royal College of Psychiatrists now accept these drugs can cause dependence and can be difficult to stop. In practice, this means some of the nervous problems patients bring to their family physician will be breakthrough anxiety and depressive symptoms, which are confronting for all concerned.
Each family doctor may only have a few cases like this, but where several doctors refer to the same psychiatrist s/he may end with many cases and no easy solution to offer. Switching to other antidepressants or adding meds is not a reliable answer and often causes further problems.
It can be difficult to offer a clear management plan. The patient’s agreement to any plan is important especially if they are likely to be faced with withdrawal difficulties. Opening up a space, therefore, where the patient, supported by a family doctor, can disagree with the ‘expert’ is important in these cases.
Family Doctor Centred
Family doctors complain specialists rarely consult them on a case. With every referral, I messaged family doctors to let them know there was an entry in the medical record. These entries often called for their input and made clear I was willing to engage further. Some doctors phoned. Many messaged back thanking me for the entry to the record and in some cases explicitly agreeing where for instance I had not supported an ADHD diagnosis.
ADHD diagnoses were never turned down flat. An alternative – you are extraverted and creative and stimulants risk inhibiting this – was offered.
Nevertheless, some family doctors may have been concerned that a willingness to recognise adverse effects caused by prior treatments might cause them problems should there be a complaint.
There is a difficult area here between the pragmatic ‘give us a view that will help us move this case forward’ and the medico-legally concerned ‘give us a view that has a basis in guidelines that will give us cover should things go wrong’.
Bureaucratic or Person Centred
Family physicians globally say they do not read reports from psychiatrists other than the closing diagnosis and treatment. The only person interested to read the full report is the person referred.
For over 30 years in Britain, I provided all outpatients with copies of all reports on them. These were framed with the person in mind rather than their doctor. They were light on medical jargon and where possible used the person’s own words. No doctor in 30 years complained about this and the letters were appreciated by patients.
In the new clinic, I emailed my entry to the electronic medical record (EMR) to both doctor and patient. The reports supported the courses of action initiated by family doctors, even where these had stopped working. I made it clear to the patient I would likely have taken the same approach in the first instance. Having asked about the relationship between patient and referring doctor, I phrased the report accordingly. The report invited patients to research things that arose in the interview including possible drug options and check these and other issues with their family doctor.
During this period, the services were operating in lockdown, which meant phone or video supplemented consults in addition to in-person meetings. A patent attempting to arrange follow-up appointments with other colleagues could take weeks, which was a problem for anyone having medication change difficulties.
My patients had their reports half an hour after a consult and were able to email me any time if they had problems. They were seen within hours or days. The normal bureaucratic wall between them and me was not there.
Medical Consumerism
Working two days a week, I saw over 300 referrals. I suggested a survey aimed at assessing what physicians and patients made of this new way of working.
Instead, at a meeting I only knew about 15 minutes beforehand, my input to the team was terminated. An undetermined number of doctors (2 that I know of) and patients (possibly only I), I was told, had been unhappy at an apparently insufficient offering of further diagnoses and treatments. There was no complaint of malpractice or investigation of any incident. A separate clinic at which I was working in the same way were happy for me to continue.
The system claimed to be unable to stream patients to me who might want this approach. I was told the system must have a standard approach, and at present at least some doctors and patients expect more diagnoses and treatments. The default is to medical consumerism and an adherence to guidelines for diseases rather than guidelines for people. None of the management team showed an interest in the idea that in the light of current evidence the first point in a guideline for people might be that no-one should be on more than five drugs.
Despite, growing discussion about deprescribing in University Departments, and among clinicians, in addition to patients interested to explore this option, as of 2021 nowhere in Canada offered sustainable treatment as part of its mix.
Where once access to treatment was a privilege of wealth, public health systems are now geared toward increasing access to medicines. Being able to reduce a medication burden it appears has become a privilege of wealth.
In North America referrals increasingly come from people approaching a family doctor claiming they have ADHD, ASD, or the latest fashionable diagnosis, expecting to be referred to a specialist who will confirm the diagnosis and initiate treatment.
These diagnoses can suck people in the way cults do. While some doctors will try to persuade patients that consumerism and poisons (medicines) or mutilations (surgery) are not natural bedfellows, and some patients can be persuaded, an increasing number complain if they are not given what they want. ‘We have the rating scale score, where’s our drug’?
There is a case for saying what a person demands, a person should get, and in the case of terminations of pregnancy, gender reassignment and medical assistance in dying, Ontario Courts have said that doctors unwilling to support these options must make an effective referral or consider switching to a non-medical career – hairdressing has been mentioned.
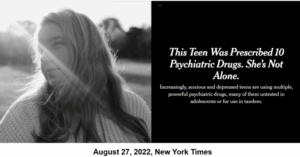
If we standardize processes to the point where everyone gets the diagnosis they want, based on rating scales they self-administer, we will end up with diagnostic and prescribing cascades, as demonstrated in the following example.
A brief upswing of mood diagnosed as bipolar disorder will lead to a mood-stabilizer, ultimately several, one of which will be an antipsychotic. When asked in clinic how they are, any mention of loss of focus, which antipsychotics are designed to produce, risks leading to an ADHD scale and diagnosis and prescription of a stimulant. A dopamine agonist is now chasing a dopamine antagonist, and both can produce depressive symptoms, leading to further antidepressants.
This is not an invented scenario. It was common in this clinic and a year it was splashed all over both The New York Times and New York Post.
Medical consumerism hinges on the idea that medicines are sacraments (can do no harm). On this basis, the managers who run health services are increasingly turning to cheaper nurse and pharmacist prescribers. We have reached a point where professional discretion is no longer valued.
Pandemic
The turn to virtual consults as a result of the Covid pandemic may aggravate these risks. Gone is the feel for someone else from a look or body language that may convey a message at odds with a patient’s words, especially when treatment is going wrong. This is a good reason for increased liaison between specialist and a primary care physician who is more likely to have laid eyes on the person before and to know how much their demeanor and deportment now differs.
The switch to new ways of working triggered by the pandemic has already led to more prepping of patients with questionnaires that shape later clinical interactions and diagnoses. An increasing number of clinical evaluations and treatment recommendations come from out-of-state doctors often through phone apps.
Our oversight of who is delivering care and the conversations between family doctors, patients, and mental health personnel necessary to good care are slipping away.
Rotten Barrel?
This state of affairs would have been inconceivable a few years ago. It stems directly from a ghost-writing of the medical literature for on-patent drugs and a total sequestration of clinical trial data. This change has confirmed the medicines in common use as sacraments. The magic of medicine once lay in the doctor who brought good out of the use of a poison, but the magic now lies in pills and doctors risk being swept away in the rush to get sacraments.
The traditional script for rooting out unethical practice will only make this problem worse by reassuring both doctors and patients that a problem has been found and the barrel is now safer than it was. We have a system problem with no clear solutions.
This wording of this post does not reflect how wild the scenario described was/is. The wording is mild because it was important to get a peer reviewed article published and this was something new for any journal – See Reducing Medication Burden.
There are other things that were happening around this time, which it may soon be possible to say something more about.
These more hard-hitting RxISK posts touch on similar themes.
- The Future of Health App-ointments
- Over-Diagnosing or Under-Diagnosing
- Repairing Ruptures in Clinical Care
- Challenging My Doctor to Disclose
Standardizing Psychiatry
Later that year, I gave a talk at a Royal College of Psychiatry Meeting covering the History of Psychiatry from 1960 to 2010. This was based on a hard-hitting book chapter in Mind State and Society that the books editors seemed to appreciate.
The audience at this talk, that I gave by video-link from Canada, included some of the luminaries of UK psychiatry. They were not so appreciative. I revisited See:
One of them said the talk posed a blood pressure hazard. Looking back at it now, it seems very very mild. Peter Selley thought so too and emailed this cartoon.
It may point to a difference between the Irish and the English. The English put things between lines and into tones of voice. Something that sounds mild to others can be read by other English as savage. Something that seems mild to an Irish person like me can be read by an English audience as wild – and maybe a Canadian one also.
The question the talk ends with is – are we creating a generation of doctors who, like salt when it loses its savor, are only fit to be thrown out?


One of them said the talk posed a blood pressure hazard. Looking back at it now, it seems very very mild. Peter Selley thought so too and emailed this cartoon.
What’s wrong with you?
A seemingly innocent question, but if the tone changes to hostile ‘What’s wrong with you? becomes the danger that innocent victims might not acknowledge.
Whether Irish, or English, Scottish, or Canadian – choose your roots and choose your language.
The question the talk ends with is – are we creating a generation of doctors who, like salt when it loses its savor, are only fit to be thrown out?
Doctors are not responding to all possibilities, they live in an Ark, the animals went in two by two. Doctors risk desrisking patients own narratives at a cost to the whole medical establishment.
‘The comments brought out how we now have a system that gaslights both patients and doctors leading to tensions on all sides as this post illustrates.’
Tensions on all sides leads to violence and death, so we come back to the cartoon, What’s wrong with you?
For readers of this comment, you have to look at the linked post and its lecture slides to see the cartoon and where the What’s wrong with you slide comes from and the irony involved.
D
An inspirational concept of a truly Person-Centred, Specialist, compassionate, expert Health Care Service.
Patient Agreement dependent, and a service that is a therapeutic experience in its own right.
What a tragedy that any Primary Care Physician could fail to support and welcome such commitment and innovation.
Tim
Thanks Tim for this. The events were mystifying at the time. I was being told that my care was excellent and a lot of people would pay for the privilege but I was being let go from a public service because folk want diagnoses and medicines and some family doctors support them in this want.
I was left casting around for the ‘real’ explanation. One possibility was I had given a lecture a week before on The Enduring Sexual Effects of SSRIs – see Sex and Evidence Based Medicine on this blog from February 12, 2021. This did get a few people hot under the collar because of its challenge to EBM. It also got some hot under collar because of one slide – which deliberately borrowed from Donald Trump’s playbook on how to grab attention.
There was another profound factor that may have played into all this – which I hope to be able to talk about soon.
But my guess is the main reason was the so unbelievable one put as bluntly as it was – as the guys who let me go said – Medical Consumerism rules – at least in Ontario.
Time was if you were chucked out of a job in Toronto’s backyard, McGill would have raced in brandishing a contrast – but not anymore
David
“In North America referrals increasingly come from people approaching a family doctor claiming they have ADHD, ASD, or the latest fashionable diagnosis, expecting to be referred to a specialist who will confirm the diagnosis and initiate treatment.”
the point is passed where a physician’s or another representative of medical authority’s word was needed for a patient to submit to any ‘necessary’ treatment. now, patients themselves are the ‘authority’ or more properly, carry the voice of the ultimate authority. mediators can be dispensed with. this development might be the end of medicine as understood until today; a unique art and science with a limited both real autonomy. just as you don’t need the advice of an expert to buy detergent, you neither need a diagnosis by a doctor to get a bottle of prozac. medicine is an obsolete art.
I am on SSRI first and then SSNI for 30 years and I have suicidal ideation, anxiety, behavioural disregularion. I weaned down to 20 mg from 250 mg over 2 years. When I stopped I had a terrible reaction. Can I use nicotine to relieve the withdrawl symptoms?
Maureen
I don’t know. There is no great reason to think it will help but if you use it and it helps, please let us know.
David