See previous posts – Switch on Anti-Depression Today and So Long and Thanks for all the Serotonin.
In response to the recent BMJ editorial on Serotonin and Depression, there were seventeen letters of which three were published, along with my response. These are copied below along with the best letter – by Barney Carroll – which wasn’t published. Make your own mind up as to why.
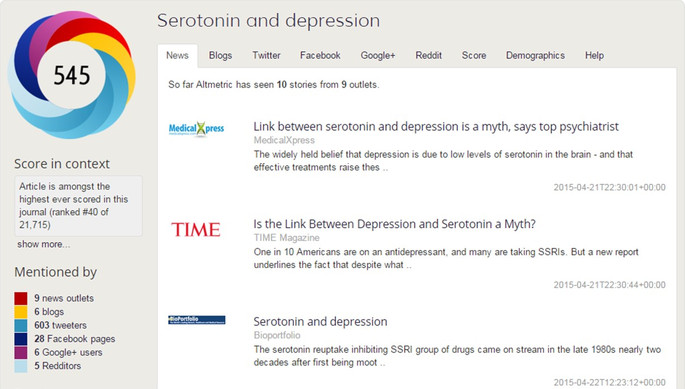
Another piece of minor intrigue is that this editorial, originally entitled So Long and Thanks for all the Serotonin, a title BMJ felt uncomfortable with, registered well on Altmetric – an index that tracks how much Buzz an article is generating. When I started looking at this, the article was rated at 43 on Altmetric and then moved down to 40 passing through 42 en route. It will presumably pass back through 42 at some point as it gets displaced by Buzzier pieces. Amusing given the Hitch-Hiker link.
Healy states the obvious
As a matter of clinical science, the notion of a simple serotonin deficiency in depression ended 45 years ago, when the proposed therapeutic utility of monoamine neurotransmitter precursors was disconfirmed.1 There has been little incisive progress since then, owing to major missteps in the intervening years – for starters, the foolish introduction of generic major depression in lieu of clinically differentiated types of depression as the focus of investigations;2 the displacement of disinterested clinical science by corporate experimercials;3 the corruption of journals and of educational forums by key opinion leaders who promoted corporate marketing narratives;4 and the capture of research funding agencies and regulatory agencies by commercial forces. The discomfort that David Healy’s editorial has caused in some quarters reflects a general embarrassment at the emptiness of current research in mood disorders. The yield has not been commensurate with the billions of dollars thrown at the problem – to the point where most corporations have exited the field out of a healthy self-interest. Little wonder, then, that those who have reason to be embarrassed are now throwing the book at Dr. Healy for stating the obvious.
REFERENCES
1. Carroll B.J. Monoamine precursors in the treatment of depression, in «Clinical Pharmacology and Therapeutics» 12, 743-76 (1971).
2. Carroll B.J. Bringing back melancholia, in «Bipolar Disorders» 14, 1-5 (2012).
3. Carroll B.J. Sertraline and the Cheshire cat in geriatric depression, in «American Journal of Psychiatry» 161, 1145-1146 (2004).
4. Carroll B.J., Rubin R.T. The high cost of non-disclosure, in «Clinical Psychiatry News» 34(10), 27 (2006).
Bernard Carroll
Serotonin and depression – Healy does a disservice to psychiatrists
Alexander E Langford, South London and the Maudsley NHS Foundation Trust
David Healy does a great disservice to jobbing psychiatrists with this editorial. By portraying them as ‘co-opted into a myth’ about low levels of serotonin being the sole cause of depression he paints them as gullible, and by stating that the same theory is ‘an easy shorthand for communication with patients’ he paints us as lazy and reductionist in our appraisal of the complex and diverse causes of depression.
In reality, good psychiatrists are and always have been only too ready to admit that they are unsure how antidepressants work. Serotonin does play an important role – likely via factors like neurogenesis and gene expression downstream from synapses – but modern psychiatry is way ahead of where Healy seems to think it is. The picture is far more complex. The fact that ketamine has been shown to be useful in depression does not ‘cast doubt on the link between serotonin and depression’, it rather confirms that the neurobiological underpinnings are as multifaceted as we think.
In any case, whatever their mode of action, SSRIs do work. Even the most stringent of analyses (i.e. Kirsch) support this. There is no good evidence that SSRIs work any less well than TCAs for depression , and the SSRIs have not become so commonplace in clinical practice due to some form of pharma-doctor conspiracy, as Healy would suggest, but because the older TCAs have a far less admirable side-effect profile and were also lethal in overdose. The safety of our patients should always come first, and they are far less safe without treatment for their depression.
Healy D. Serotonin and depression. BMJ 2015;350:h1771. (21 April.)
Serotonin and depression: myth or legend?
Philip J Cowen, Professor of Psychopharmacology, University of Oxford,
David Healy’s observations on serotonin and depression make interesting , if familiar, reading [1]. However, I was struck by the remarkable claim that the focus on serotonin has led to the ‘eclipse of cortisol’ in mood disorder research. A quick search in Scopus with ‘cortisol’ and ‘depression’ revealed a rapidly increasing number of published articles from the late 1990s, continuing unabated to the present time. Only last year saw the completion in the UK of a large placebo-controlled study which examined the effects of inhibiting cortisol synthesis in patients with depression refractory to SSRIs[2]. David also manages to suggest that ketamine has been shown superior to SSRIs in melancholic depression whereas no such comparison has been carried out. He further implies that the work of Andrews and colleagues is based on the intellectually paralysing notion that low serotonin causes depression whereas in fact these authors argue exactly the opposite [3].
Should one confront myths by constructing different ones? As an avid BMJ reader I find myself increasingly confused by this question. For if scientific narratives are manifestations of competing power claims and vested interests perhaps there isn’t really a ‘fact of the matter’- the important thing is to be on the right side. I agree with David.
- Lacasse JR, Leo J. Serotonin and depression: A disconnect between the advertisements and the scientific literature. PLoS Med 2005; 2: e392 DOI: 10.1371/journal.pmed.0020392 (http://medicine.plosjournals.org).
- Watson S, Anderson IM, Apekey TA, et al. Antiglucocorticoid augmentation of antidepressants in depression: The ADD study. J Psychopharmacology 2014; 28 (suppl): A38.
- Andrews PW, Bharwani A, Lee K R, et al. Is serotonin an upper or a downer? The evolution of the serotonergic system and its role in depression and the antidepressant response. Neurosci Biobehavior Rev 2015; 51: 164-188.
Serotonin and depression – personalized pharmacotherapy: an interim solution?
Adam M Chekroud. Yale University, USA
Prof. Healy offers an engaging historical perspective on the rise of serotonergic antidepressants that questions their efficacy and biological plausibility. However, this focus on low serotonin levels is a distraction that is basically irrelevant to whether serotonergic antidepressants are effective treatments for depression. It is important to note that response to serotonergic antidepressants appears to be heterogeneous rather than universally poor. Unbiased trajectory-based analysis of over 2500 patients treated with SSRI antidepressants or placebo indicated that the majority of patients (over 75%) showed a superior response to patients treated with placebo. However, nearly one quarter of patients treated with SSRIs showed a poorer response than patients treated with placebo. This suggests that in these patients, SSRI treatment actually interferes with their capacity to mount a placebo response, or perhaps even their capacity for resilience to depression [1]. This raises the critical issue of whether there are ways to identify those patients who would seem to be better off avoiding SSRIs and to divert these individuals to other treatments for their depression.
One factor reducing the effectiveness of antidepressants treatment is our inability to personalize pharmacotherapy, i.e., clinicians have no mechanism for predicting whether a particular patient will respond to a specific antidepressant. Instead, the process of matching patients and treatments requires a prolonged period of trial and error, delaying clinical improvement and increasing the risks and costs associated with treatment. Despite important progress in trying to identify depressed patients at high risk of treatment resistance [2], Psychiatry continues to lag behind other specialties like Cardiology and Oncology in which personalized treatment selection is far better established [3,4].
Developing more generally effective treatments and more rapidly effective treatments would be extremely important advances for public health. However, in the absence of any such silver bullet, we advocate the development and implementation of innovative statistical methods to get the best available drug to each patient, as an interim solution. Personalized pharmacotherapy may still enable us to “save lives and restore function”. Giving up on these patients is not an option.
- Gueorguieva R, Mallinckrodt C, Krystal JH. Trajectories of Depression Severity in Clinical Trials of Duloxetine: Insights Into Antidepressant and Placebo Responses. Arch. Gen. Psychiatry. 2011;68:1227–37. doi:10.1001/archgenpsychiatry.2011.132
- Perlis RH. A clinical risk stratification tool for predicting treatment resistance in major depressive disorder. Biol Psychiatry 2013;74:7–14. doi:10.1016/j.biopsych.2012.12.007
- Kumbhani DJ, Wells BJ, Lincoff AM, et al. Predictive models for short- and long-term adverse outcomes following discharge in a contemporary population with acute coronary syndromes. Am J Cardiovasc Dis 2013;3:39–52.http://www.ncbi.nlm.nih.gov/pubmed/23467552
- Roobol MJ, Carlsson S V. Risk stratification in prostate cancer screening. Nat Rev Urol 2013;10:38–48. doi:10.1038/nrurol.2012.225
A pleasing look of truth
I wrote an almost identical editorial as this in 1991 (1). Covering the marketing of serotonin in 1997 (2), I cited Jerome Gaub’s 1767 opinion of Leibniz’ views on the relations of the mind to the body – it is a “fable whose novelty has recommended it, whose recommendation has spread it, whose spread has polished it, refined and adorned it with.. a pleasing look of truth” (3)
I use SSRIs. Nevertheless I believe the SSRI era will soon stand as one of the most shameful in the history of medicine. The shame does not stem from what pharmaceutical companies have done, which is just as might have been expected. The shame will be seen to have arisen from the failure of doctors to know as much as they should have done about medicines they dish out so liberally. A recent study showing how a dollop of neuroscience dressing can disguise otherwise meaningless material should be compulsory reading for doctors who are after all the true consumers of these drugs (4).
But perhaps an even greater shame will be seen to lie with the fact that this has been an era in which the bulk of publications on on-patent drugs in our best journals were ghostwritten, an era in which the journals refused to demand access to trial data as the price of publication – nowhere more clearly demonstrated than in the area of antidepressant studies on children. It has been an era when industry has controlled journals, by spending money on some of them and by intimidating others into self-control.
- Healy D. The Marketing of 5HT. British J of Psychiatry, 1991; 158, 737‑742.
- Healy D. The Antidepressant Era. Harvard University Press, Cambridge Ma 1997.
- Rather LJ. Mind and Body in 18th Century Medicine. Wellcome Historical Medical Library, London, P 17. 1965
- Weisberg DS, Keil FC, Goodstein J, Rawson E, Gray JR The Seductive Allure of Neuroscience Explanations. J Cogn Neurosci. 2008; 20, 470–477.
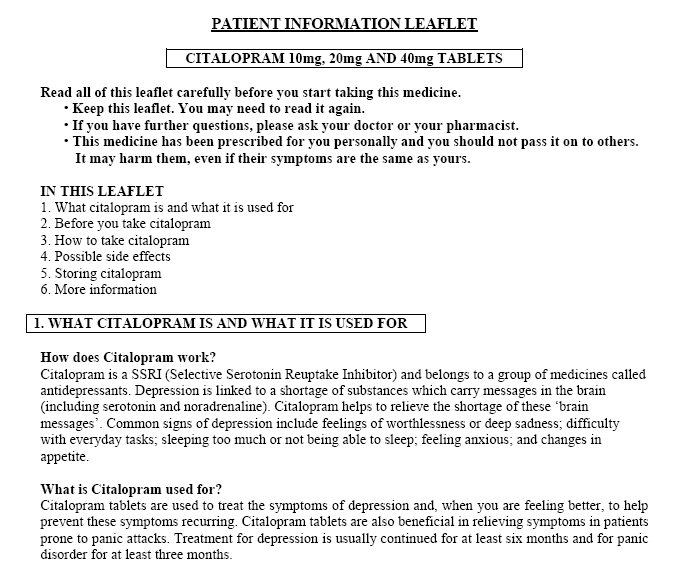
Meanwhile the patient information leaflets for pretty well all antidepressants and wannabe antidepressants like quetiapine as of today continue to promote versions of the Low Serotonin Hypothesis (thanks to Julie P for pointing this out).
This should incense a lot of people.
Nevertheless I believe the SSRI era will soon stand as one of the most shameful in the history of medicine.
I agree with this quote totally, and the problem at the present time is how to help people who have become victims of the lies of SSRIs, and are suffering all hell after having used them. How do I get back to the day before I ever took the poisons? How? Help me? Someone?
Go to theroadback.org website and read their materials.
GVK Biosciences is the latest Indian firm to come under international scrutiny over quality issues. Several large Indian drugmakers have over the past two years faced U.S. and UK sanctions over issues ranging from data fabrication and manipulation, to sanitation.
Yep read the report, the audit done by France on behalf of the European Union.
Guess the compliance? The rate of traials that were genuine, verifiable? Not too hard to guess 10% passed, ie 90% of 3,000 trials were fabricated,.
http://www.reuters.com/article/2015/04/15/gvk-bio-india-idUSL4N0XC1O320150415
Alexander E Langford from Maudsley NHS Foundation needs to wake up and get real. His comments are deeply misguided and insulting to both Dr Healy and patients alike. “A great disservice??” What planet is this man on? He writes “In reality, good psychiatrists are and always have been only too ready to admit that they are unsure how antidepressants work” (I think this is supposed to reassure us) He then goes on to deliver perhaps the greatest insult to patients ” The safety of our patients should always come first and they are far less safe without treatment for their depression.” How short sighted and what a generalisation! What hope is there for psychiatry when someone who claims to care about patient safety describes the man at the helm of common sense and patient care as doing psychiatry a disservice?! How can you say with such conviction Mr Langford that “SSRIs do work” if you admit you do not know how they work? Some people may be made better by drug intervention but not everyone all the time. There are many factors at play in someone’s treatment, to say someone is better on a drug than without it, well that depends upon a number of factors. This is another example of a one size fits all approach which offers no wriggle room for those who have genuine concerns about treatment. He says on his blog that he is “interested in changing the public face of psychiatry.” I for one would be very interested if Mr Langford could tell us how exactly he intends to do that.
I Concur with Sarah. Why Is It That Many Psychiatrists Keep saying, “The SSRI’s Are A Better choice For Depression Because They Are Safer Than The TCA’s In An Overdose.” They Don’t say, “SSRI’s Have Been Proven Superior To Placebo and In Many Cases Superior and/or Better Than TCA’s.” Isn’t The Dr. Supposed to Write the Script for The smallest Number Of Pills, Say in This Case a Weeks worth. It Sounds to me as if everyone who receives A TCA or MAO Are Taking These Pills Left and Right. Use A TCA Or MAO and Just call in more Tabs Once a week Or Until The Patient is feeling much better. To give the reason that The Major reason for Using Or Not Using a Drug Is because one set Of drugs Is safer If You should feel the need to take the Whole bottle is Hilarious to Me. The reason why one set of drugs Should Be Used Over another Should Be Because it Gets The Patient Well, Back to The swing of Things, Back to work Or School. Wanting to be with family and not sleeping all day long. In This Case The TCA’s Are A Better choice because of Efficacy. I was On Tofranil in 1989-1990. Prozac was available then, but My Dr. Chose Imipramine Because of Anxiety along with depression. After 6 weeks I was Discharged With A script For Tofranil. I took it for many months and did feel better in terms of less anxiety. We Used TCA’s For Many, Many Years Before the SSRI’s and The Majority Of us Have come Out For the Better. If One does Try to kill themselves With A TCA It more than likely will be the last time They do That. Not Because they are Dead but Because They are Going To Get Very sick and Have invasive procedures performed on them. I Do Feel Though that Psychiatrists Do Care and Look Out For Their Patients, At Least Mine does. Psychiatry is a hard branch of Medicine to cope with because medicines and treatments are put through the ringer a lot of the time. This low 5-HT nonsense has got to stop though. We Need to just say that we really do not know what causes or why some people get seriously Depressed but I’m not Going To Stop looking for an answer. Dr’s Need to start listening more to their Pt’s When describing a particular feeling, Good or Bad that they feel a drug is causing. I certainly would. We can learn so much if we really investigated the Pt’s Concern. Nothing Is set in stone when it comes to a drugs effects or lack of one. I really have learned a lot from Dr. Healy. His Books Are Very informative, So are his lectures. Doctors don’t always know more than their patients. We Have a mental illness but we are smart and able to form logical questions to a set of given problems. I really feel that some Dr’s feel that because This person has a mental illness he/she cannot look at a particular problem in a scientific manner. I know my GP is like that and it’s too bad. Psychiatrists are a great bunch of people. The ones I Know are kind, like to throw out a good joke and respect the mentally ill and people in general. Thanks For Reading.
Far be it from me to contradict the experts, but is the BMJ itself contributing to the myths and fallacies of the unbalanced chemical basis of depression? Selectively choosing which comments are published to suit an objective. It’s interesting that Bernard Carroll’s comment went unpublished when the critiques by Prof Cowen et al were permitted.
In the following paper Prof Cowen states “there is now substantial evidence that unmedicated depressed patients have abnormalities in brain 5-HT (serotonin) function..” This is absolutely untrue and helps to push the ‘chemical imbalance’ myth.
http://www.ncbi.nlm.nih.gov/pubmed/18585794
If the BMJ are going to selectively choose which comments are published, it is surely their responsibility to also ensure that the information provided is factual and from evidence-based sources. I’m sure David Healy must be bored by now at the same people ‘having a go’ at every possible opportunity. The BMJ should distance itself from it.
WHY THE BMJ PICKED THESE 3 SPECIFIC LETTERS FOR PUBLICATION: A HYPOTHESIS
I am not well-versed in psychopharmacology but am very well-versed in being prescribed psychotropic drugs, including almost all SSRIs since their inception, along with the universal reassurance from well-meaning doctors (whom I respected as knowing more than myself) that the drugs correctedtargetedin some way acted on serotoninchemical imbalance.
So I’ll stick to what I do know: the art of language, semantics and reasoning.
Why these three letters? Why not Bernard Carroll?
The ‘Short Answer’, as I see it: The published letters plausibly and neatly distract from the primary purpose of David Healy’s article, i.e. the SEROTONIN/SSRI MESSAGE/MYTH AND ITS MARKETING.
(Although related and important it wasn’t primarily about effectiveness, other theories, causes of depression, Public Health).
Why I came to this conclusion is in the ‘Long Answer’ below.
BMJ cannot ignore the amount of interest and comment the article has stirred.
BMJ cannotwill not (?) upset the established apple cart. Why? Not for me to speculate.
Methodology: skilled use of ‘the science’, ‘Hearts and Minds’ and the logical fallacies inadvertently put out by the authors of the letters. (If I’ve fallen foul of any of these hard-to-avoid logical traps, corrections graciously accepted.)
Format: Taken together the 3 letters strangely remind me of a French dissertation rather than 3 separate letters (selected in the interests of openness and fairness?)
Letter 1 – the People’s Psychiatrist. Emotive vocabulary (viz. ‘gullible’, ‘lazy’, ‘good’, ‘paints us’), smatterings of ad-hoc reasoning, a touch of subtle ad hominem, straight in with the ‘Hearts’ bit so that even the glaring inaccuracies in the letter are hard to spot.
Letter 2 – the ‘Friendly Fire’. Referential language but serious dose of ad-hoc reasoning by focusing on anything in David Healy’s article (i.a cortisol, ketamine) except the serotonin, thus distracting and casting potential doubt on David Healy’s conclusions re Serotonin (remember, the primary point of the article).
Letter 3 – provides the coup de grace. By far the longest of the three. Elaborates and develops on Letter 2 with more distraction (studies, other specialties, Public Health, personalised pharmacotherapy). And who said anything about giving up on patients?
The letters make some perfectly valid points. But now, Dear BMJ Reader, you’re not only confused about the ‘science’ bit but you’ve also probably forgotten what the article was primarily about.
Sterling job, BMJ!
DECLARATION OF INTERESTS: NONE, APART FROM MY OWN SANITY
Julie
Brilliantly written comment Julie. Summed it up perfectly.
Language, semantics, and reasoning… are truly beautiful. Great job!
An important question for everyone is:
Are the drugs on trial?
Or
Are the writers on trial?
The BMJ have stated that Pharmaceutical companies should not be in charge of their own drug trials.
The BMJ have allowed writers to pontificate as ghost writers.
Is it possible to redact BMJ articles published
Or
Once published is the damage done
Maverick, Radical, Gadfly are words bandied about with little thought for the recipient
Or
It is intended that the recipient might kowtow
Agreed, Leonie! It might be refreshing to see a Trainee like Alexander Langford published in the BMJ … until you realize they declined to publish Bernard Carroll, and also didn’t feel other letters from “junior doctors” were worthy.
Like this one from a very recent grad:
“Throughout medical school the doctrine of neurotransmitter imbalance, in particular Serotonin, was the gospel explaining the pathophysiology of Anxiety and Depression as one disease.”
Or this from a humble GP:
“I feel embarrassed that I, like most GPs have been persuaded that I should encourage patients to take medications for which the benefits are so poorly shown. How is it that this information is only becoming available after the SSRI patents have expired?”
GPs do most of the actual prescribing of these pills. How far up the food chain does one have to go before being admitted to the chummy club where “everyone knows” that simplistic theories of chemical imbalance hit the wastebasket long ago? Your doctor and mine don’t rate, I’m afraid.
All the Rapid Responses to David’s editorial can be read here (for now):
http://www.bmj.com/content/350/bmj.h1771/rapid-responses
The ad For Celexa is Definitely Far Out There. It Almost reads As though The Makers of That Crap, Citalopram, Are Speaking To a Bunch of First Graders. Citalopram Helps to “Releive” The Shortages Of These Chemicals. Why Leave It At That??? Please Explain To Us How Our Good Friend Citalopram Does This Miraculous Work.
Is It like A Space Ship Or A Creature From A Far Away Planet Honing In On The Shortage Of Chemicals. Or Is Citalopram a Bit Like Whats Her Face On “Bewitched”
Shrinks Wiggle Their Nose at Their Pt’s and All Is Well. No More Chemical Shortage. That’s A Good trick. I Wish My Dr. Whom I Have a lot Of Respect For Would Pull This Rabbit Out of Her Hat. And I would Ask Another Thing! How did I Come About Getting This Little Chemical Imbalance??? And What Do They Mean By Chemical??? Can I Have The molecular Structure Of This chemical please?? Here We Go Again With The Pharmaceutical Co’s Talking Down To Those Of Us Who Have This Imbalance. We Can and Do Under Stand High Tech Sophisticated Words and Sentences. Perhaps The Imbalance is Supposed To Make Us Dumb. Citalopram=Dry Mouth, Weight Gain, Somnolence, Indifference To Surroundings and/or Environment, Insomnia, Hypersomnia, Myopia, Diarrhea and/or Constipation, Urinary Hesitancy, Delayed Or Lack There Of Orgasm. Growing Lack of Concern or Interest for Sex, Music, Love, Friends and Family, School, Foods Once Loved, Disinterest in Intimacy and/or Closeness With Significant other. Need I go On. Kind Of Sounds a Bit Like That Other Miracle Drug Abilify That I saw Willy Wonka Pushing Instead Of Everlasting Gobstoppers.
“However, nearly one quarter of patients treated with SSRIs showed a poorer response than patients treated with placebo. This suggests that in these patients, SSRI treatment actually interferes with their capacity to mount a placebo response, or perhaps even their capacity for resilience to depression.”
That is an ingeniously round-about and euphemistic way of saying that SSRIs make some patients worse, rather than better!
But this has always been obvious from the fact that the average benefit of SSRI treatment in depression trial reports is small to zero in magnitude, but the scatter around the average outcome is large. In other words, the proportion of patients who benefit is at most only slightly larger than the proportion who get worse.
One group made worse by SSRIs are probably those whose depressed mood is due to reduced affect/ anhedonia – and whose lack of emotional responsivity is worsened by SSRIs (this being the core effect of SSRIs)
D. Nutt, K. Demyttenaere, Z. Janka, T. Aarre, M. Bourin and P.L. Canonico et al., The other face of depression, reduced positive affect: the role of catecholamines in causation and cure, J Psychopharmacol 21 (2007), pp. 461–471.
Marketing the myth of serotonin, the ‘happy chemical’
ADRIANA BARTON – The Globe and Mail
If serotonin is the “happy chemical,” then boosting our serotonin levels should keep depression at bay. After all, low serotonin brings on the blues, right?
But the truth is, depression is not a serotonin deficiency. The idea that depression is caused by low serotonin levels is based on flimsy evidence dating to the 1950s. Pharmaceutical companies promoted the low serotonin story to sell Prozac and related antidepressants. They marketed a myth.
Today, the serotonin fallacy is as ingrained as the notion that drinking orange juice wards off a cold. Many of us still believe we are raising our serotonin levels to lift depression using wildly popular drugs known as selective serotonin re-uptake inhibitors, or SSRIS. But psychiatrists now say it is unlikely these drugs treat depression by simply increasing serotonin. While antidepressants help many patients, researchers have only a hazy idea of how they work.
The consensus is that depression is a complex disorder with hundreds of potential underlying causes, said Dr. Roger McIntyre, head of the mood disorders psychopharmacology unit at the University Health Network in Toronto. “There’s really no scientific case to say that people who have depression have a deficiency in body and brain serotonin levels.”
The medical journal BMJ put the spotlight on the low serotonin doctrine in a recent editorial published in April and written by Dr. David Healy, a professor of psychiatry at Bangor University in Wales.
Blockbuster sales of antidepressants such as Prozac are based on the marketing of the serotonin myth, Healy wrote. He added that pharmaceutical companies misled the public into putting too much faith in SSRIs.
Scientists never confirmed whether SSRIs raise or lower serotonin levels. “They still don’t know,” Healy said.
Many of his peers suggest that Healy is not a respected figure in psychiatry, in part because of his stance that older tricyclic antidepressants are better than today’s Prozac-type drugs. His colleagues maintain that SSRIs are safer if taken in overdose than older antidepressants, and caution that patients should not switch medications based on Healy’s views.
Nevertheless, most psychiatrists agree that depression is not a matter of serotonin levels being up or down. The role of serotonin in depression is best described as a “dysregulation” of the serotonin system, McIntyre said.
The serotonin system regulates aspects of behaviour, thought processes and mood. But it also interacts with other brain systems that may be involved in depression.
Modern antidepressants block the re-absorption of serotonin in the brain. When researchers discovered that SSRIs helped depression in some patients, they concluded that low serotonin must be the cause of the disorder. But the assumption was no more valid than the notion that “having a headache means that your Tylenol levels are low,” McIntyre said.
McIntyre described psychiatrists as being “guilty of exuberance” when they framed depression as a low serotonin problem.
But others, including Healy, point fingers at the pharmaceutical industry. Starting in the late 1980s, Prozac and other “miracle pills” promised to treat serotonin deficiency as easily as vitamin C cures scurvy.
Marketing materials for the new antidepressants presented the unproven low serotonin hypothesis as fact, according to a 2005 study in the journal PLOS One.
For example, on a branded website for an antidepressant called Celexa, the FAQ section claimed that “Celexa helps to restore the brain’s chemical balance by increasing the supply of a chemical messenger in the brain called serotonin.”
Doctors adopted the low serotonin story as “an easy shorthand” for explaining depression to their patients, Healy wrote. Patients were receptive to SSRIs because the idea of correcting a chemical imbalance reduced the stigma of mental illness.
Treating depression with Prozac was reportedly a cinch. “You can teach a chimpanzee to prescribe it,” a psychopharmacologist was quoted as saying in a 1989 New York magazine cover story entitled Bye-Bye Blues: A New Wonder Drug for Depression.
But the hype did not prepare patients for side effects ranging from nausea and anxiety to suicidal thoughts – or the strong chance that SSRIs might not relieve their suffering.
Two out of three patients with depression either do not respond to SSRIs, or get only partial relief on SSRIs and other antidepressants, according to findings from STAR*D, the largest clinical trial study of depression medications. Completed in 2006, the trial was funded by the U.S. National Institute of Mental Health.
When SSRIs work, improvements in depression may be due to direct action on the serotonin system, or downstream effects of serotonin on other systems.
For example, severe depression is a side effect of interferon, a drug prescribed to spur the immune system in patients with skin cancer and Hepatitis C. Studies have shown that preventive treatment with SSRIs greatly reduces the risk of depression in patients on interferon. Based on these findings, “clearly the serotonin drugs have indirect effects on the immune-inflammatory system,” McIntyre said.
The fact remains that not all patients benefit from taking SSRIs. Thus, the logical conclusion is that the right treatment depends on the individual cause of the patient’s depression, McIntyre said. Depression is an illness of the brain – “by far the most complicated organ in the human body,” he pointed out.
Treating depression may never be as simple as prescribing insulin for diabetes or ibuprofen for fever. And despite what pharmaceutical marketing may say, no single pill can cure this ill.
Antidepressant marketing
The marketing of antidepressants is worth a second look, since history tends to repeat itself.
Right now, the top-selling drug in the United States ranked by sales is Abilify, a powerful antipsychotic. Sales took off in 2007 when the drug was approved as an add-on treatment for depression in patients who do not get adequate relief from taking an antidepressant alone. (Canada approved this use in 2013.) By March, 2014, annual sales of Abilify topped $6-billion.
U.S. advertisements for Abilify say the drug works “like a thermostat to restore balance.” But the drug’s product insert acknowledges that the mechanism of action “is unknown.” As with antidepressants, researchers have no idea how Abilify works.
In fact, psychiatrists are just beginning to understand what causes depression and why medications work for some patients, and not others.
Some researchers hypothesize that depression is due to a dysfunctional glutamate system. Disruptions in this fast-acting signalling system may alter neuroplasticity, the brain’s ability to change and adapt in response to stress and other events. Reduced plasticity may lead to depression.
A second theory, known as the metabolic hypothesis, suggests that insulin, like glutamate, facilitates brain plasticity. Depression may occur when brain regions do not make enough insulin or cannot respond to insulin properly.
Other researchers are testing the immune-inflammatory hypothesis – the idea that depression is caused by inflammation due to an overworked immune system.
Another line of thinking, known as the bio-energetic hypothesis, suggests that tiny powerhouses within brain cells may not be producing or disposing of energy and energy byproducts properly. This may lead to destruction of brain cells, and consequently, depression.
All are “very active” areas of research, McIntyre said, “and they are not mutually exclusive.”
1) Barton got stuff right out of the initial SMC expert reactions:
[Healy is routinely bashed by the true believers] “…because of his stance that older tricyclic antidepressants are better than today’s Prozac-type drugs. His colleagues maintain that SSRIs are safer if taken in overdose than older antidepressants, and caution that patients should not switch medications based on Healy’s views.”
Those reactions were like a caricature, a Monthy Python skit. I tried to convey that in my (newly revised) blog post.
“Wessely led the charge, apparently having shot his wad long before reaching the fray. Not one to skip a gunfight for lack of ammunition, he gave it his paltry all with “antidepressants are helpful in depression, together with psychological treatments…”
https://evidencer.wordpress.com/2015/05/13/when-psychiatrists-implode-panic-hysteria-and-narcissism-or-just-drunk/
2) Julie I see a future for your work…Journal of Meta-pharmacology
Alexander Langford: David Healy does a great disservice to jobbing psychiatrists with this editorial.
But he gives a great service to the people who have to suffer the horrendous side effects of meds prescribed to put something right that never existed in the first place.
Oh I agree, well said LISA….. Oh how we suffer, if only, if only I could go back to the day before I took that poison. My life is destroyed, my marriage destroyed, my sanity destroyed.
Every newspaper has competition. The BMJ is merely a newspaper, a tabloid, if you will.
There really should be a competitor going up against the likes of these journals. Okay, we have voices – bloggers, organizations, even psychiatrists and other healthcare professionals who speak out.
What is to stop someone (or a group of people) writing a journal that offers more balance than the BMJ?
Nothing stopping them… but why? Start small, talk to your friends, be honest and open. Internet and social networking is a powerful tool, we have the unheard of ability now… we can talk to (text) ANYONE IN THE WORLD…. one on one, no editing, no nothing…… I am realising the world is a small place,……….never before in the history of mankind, have people anywhere been so freely able to communicate, without corruption, manipulation, propaganda…. one on one… communication, wow!
I vote aye, Bob.
Not a journal, Bob, – well, not JUST a journal – but a well planned and orchestrated campaign utilising all means of communication and influence open to us – and these are numerous.
The planning stage needs to commence asap before many others (like I have done) fall foul of these evil drugs. We owe it to mankind.
Who wants to join me?
Even before the concept of chemical imbalance was first formally proposed by Joseph Schildkraut in 1965 [Schildkraut, J. J. (1965) The catecholamine hypothesis of affective disorders: a review of supporting evidence. Am J Psychiatry], wiser minds in behavioral pharmacology were noting the simplification:
“The concept of humors, since it was clearly enunciated by Hippocrates, has been declared scientifically extinct at several periods of history, yet it has lingered on in such words as choleric and melancholic. In recent years there has been a resurgence of interest among biochemists in the doctrine of humors in brain and it comes in a form recognizably similar to that of the ancients. Nowadays, however, people speak of 5-hydroxy-tryptamine (serotonin) and catecholamines instead of black bile and yellow bile as related to depression and elation.”
“HUMORS”, P. B. (Peter) DEWS, Stanley Cobb Professor of Psychiatry, Harvard University, (Read April 24, 1964, in the Symposium on “Psychology: A Behavioral Reinterpretation) Proceedings of the American Philosophical Society 1964.
i.e. in 1964 the error of this gross simplification was clearly noted, along with its ancient origins. Serotonin and noradrenalin in place of black bile and yellow bile.
Here I am tap, tap, tapping my way through my comment about the BMJ when two things happened.
An email in my box from Alltrials (see email in full below) a little bit hysterical about this latest piece of news:
http://www.theguardian.com/business/2015/may/18/drug-trials-firm-to-challenge-plans-for-greater-transparency-over-results
and, then, Richard Littlejohn, one of the funniest journalists, I read, had a go at Clare…G.
http://www.dailymail.co.uk/debate/article-3087063/RICHARD-LITTLEJOHN-old-GP-think-daughter-s-scaremongering.html
What will Simon say……..?
Anyway……..
Don’t you reach a point when all the skulduggery becomes laugh a minute entertainment for all of us………..what else can you do?
Dear AllTrials supporters
We’ve just learned that progress on clinical trial transparency could be at risk. A company which conducts clinical trials on behalf of industry, Richmond Pharmacology Ltd, is launching a judicial review against the UK’s Health Research Authority (HRA), challenging the HRA’s world leading efforts to reform trial registration.
The HRA is the body set up to protect and promote the interests of patients and the public in health research in the UK. It has been working hard to make clinical trials more transparent, supported by thousands of patients, doctors, pharmacists, researchers and the public. It has made trial registration a condition of running a trial in the UK and has asked researchers who want to run trials to ensure that all trials they’ve run in the past have been registered. If the decision in the judicial review goes against the HRA, this fantastic work and all our efforts to break through the era of secrecy on clinical trials could come to an abrupt stop.
Síle Lane, Director of Campaigns, Sense About Science, co-founding organisation of the AllTrials campaign said: “It is shocking that a company is using court action to try to stop transparency. We want the HRA to help right the injustice done to the thousands of patients who have taken part in clinical trials that have been kept hidden. I find it deplorable that one company is trying to stop that.”
The news was reported today by the Guardian. As soon as we know more details we’ll be in touch. In the meantime, please share this story with your colleagues, friends and networks.
Kind regards
James
James Cockerill
Campaigns Manager
Sense About Science
Science and evidence in the hands of the public
Richmond Pharmacology sound highly professional…
http://warningagainstrichmondpharmacology.blogspot.co.uk/2009/08/warning-against-trials4us-aka-richmond.html
Walter
The Globe and Mail article is interesting. Turns out that Bristol Myers Squib were reprimanded by FDA for adverts claiming that Abilify was like a thermostat – gets the brain temperature right whatever the weather 7 years ago and Otsuka just last month were reprimanded by FDA for the same thing – using this image and claiming support from academic articles produced notionally at least by Stephen Stahl in 2001 and others afterwards:
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/EnforcementActivitiesbyFDA/WarningLettersandNoticeofViolationLetterstoPharmaceuticalCompanies/UCM443935.pdf
It’s quite something, with the dimmer switch and the brains and all …
The intriguing thing is the material showing a thermostat is aimed at doctors – it was consumers shown this idea first of all.
I react as Bruce did towards Adam Chekrouds reflections.
” 3 out of 4 becomes better with SSRI, and the 4th would too, if he had better placebo reaction”
A grown man, a scientist, with rhetoric like a 5-yearold.
How is it even possible that 75% get better on SSRI in his reference, and other science shows no efficacy?
Scrap it all, start over, even if it is immoral we need a new large scale trial.
Including people without prior history of mental disorder.
Without “washout-periods”.
And followed to every letter of the law to avoid biased results.
Follow-up must be several years.
At least stop the debate where people refer to left and right to flawed research.
The gap is statistically too wide between ‘positive’ and ‘negative’ research.
If the drug is the same, the results should end up in a very narrow gap of findings.
You don’t need a degree to understand that.
To quote the late Molly Ivins, “We have to have fun while trying to stave off the forces of darkness becuase we hardly ever win, so it’s the only fun we get to have.”
However, in my view, this is starting to change.
The truth will out, and justice will come, in my view.
unfortunately this is not Lord of the Rings – the truth can be buried for ever and is more likely to be buried than not – the only thing that can change this is if sufficient people are mobilized on the ground
DH
I am mobilized and I am on the ground and Geeta and David have both used the world *change* so Change.org seems quite relevant, today:)
I recently signed this petition as someone who is not happy with the MHRA.
If I was happy with the response I received from the MHRA in December, 2011, there would have been no need to sign this petition.
I sent them an email, see below, and, received a reply, see below.
It is up to anyone to ask if the reply I received from the MHRA was suitable – under the circumstances………………
Just something to consider….Change.org
https://www.change.org/p/house-of-commons-to-disband-the-medicines-and-healthcare-products-regulatory-agency-mhra-a-corrupt-government-body-charged-with-protecting-patients-from-avoidable-harm-in-the-national-health-service-and-in-public-health?tk=tlHqV0Fop-kWc31c-1fPojlMe8b_iS2YZX4UqhJCfJ0&utm_source=supporter_signature_milestone_email&utm_medium=email&utm_campaign=supporter_signatures_1000
Cc: MHRA Central Enquiry Point ; “Williams, Dr Julie”
Sent: Thursday, 8 December 2011, 11:29
Subject: Seroxat
Dear Ms. Bevan,
Thank you for your email describing your experiences in relation to Seroxat (paroxetine).
The issue of suicide and related events and withdrawal reactions following use of Seroxat and all Selective Serotonin Reuptake Inhibitors (SSRIs) has been monitored by Medicines and Healthcare products Regulatory Agency (MHRA) and its predecessor the Medicines Control Agency since the early 1990’s. Warnings about the risk of withdrawal reactions upon stopping treatment with SSRIs have been included in the Patient Information Leaflets for SSRIs for many years and a number of measures have been taken to raise patient and prescriber awareness of these reactions.
The Committee on Safety of Medicines’ Expert Working Group on the Safety of SSRIs included an evaluation of withdrawal reactions. Updated, authoritative and advice on management of withdrawal from SSRIs is available in the product information for prescribers (SPC) and the Patient Information Leaflets (PIL). Feedback from patients and patient organisations informed the current wording on withdrawal reactions in the PILs for SSRIs.
The current National Institute for Clinical Excellence guidance on ‘Depression: management of depression in primary and secondary care’ contains clear information under ‘key priorities for implementation’ that ‘all patients prescribed antidepressants should be informed that, although these drugs are not associated with tolerance and craving, discontinuation/withdrawal symptoms may occur on stopping, missing doses or, occasionally, on reducing the dose of the drug. These symptoms are usually mild and self-limiting but can occasionally be severe, particularly if the drug is stopped abruptly.’ It also advises that patients should be asked to seek advice from their medical practitioner if they experience significant discontinuation/withdrawal symptoms.
The British National Formulary, which is distributed by the Department of Health to doctors and communities pharmacies, also mentions withdrawal reactions following stopping treatment with SSRIs.
It is recommended that discontinuation of any of the SSRIs is gradual and not abrupt. However, one formal protocol covering the recommendations for withdrawal of all SSRIS is not published or approved by the MHRA. The half lives of the individual SSRIs vary and so the withdrawal schedule needs to be tailored to an individual drug and an individual patient’s clinical circumstance. This is something the prescribing doctor is best placed to judge on an individual patient basis and the patient and doctor should ideally discuss the possibility of withdrawal side effects.
In May 2006, prescribers were informed about a new analysis of the risk of suicidal behaviour in the adult population by the US Food and Drug Administration – the overall conclusions that review were consistent with those of the UK review – i.e. that adults who receive SSRIs are not at an overall increased risk of suicidal thoughts or behaviour but that young adults (i.e. those younger than 25 years) may have an increased risk of suicidal behaviour.
In August 2007, an article was included in the MHRA drug safety bulletin, Drug Safety Update, providing further information to prescribers about the risk of suicidal behaviour with antidepressants and advising particularly close monitoring of young adults.
Most recently discussions within Europe have led to a decision that the product information for prescribers (Summary of Product Characteristics- SPC) and the Patient Information Leaflets (PILs) for all antidepressants, not only SSRIs, should be updated to contain clear warnings with respect to the increased risk of suicidal thoughts and behaviour in young adults and the need for close monitoring of patients. This information has been posted on the MHRA website (www.mhra.gov.uk) and prescribers made aware of this via Drug Safety Update and via updates to the SPC available at http://www.emc.org.
It is considered good practice for the prescribing physician to discuss the risk and benefits of any medicine as outlined in the SPC available to all prescribers with their patients and for patients to have the patients information leaflets to take home for further reference to the key risks and to enable discussion with carers.
The safety profile of Seroxat is continually reviewed by the MHRA and the balance of risks and benefits carefully and continually re-evaluated along with the need for timely communication of any new safety information identified and updated to the product information for prescribers and patients.
If you have not already done so I would encourage you to report your experiences to us at the MHRA through the Yellow Card Scheme. Yellow cards are available directly from the MHRA: CHM Freepost, London SW85BR or electronically via the MHRA website (www,yellowcard.gov.uk).
Many thanks for your kind comments on our educational materials on the website. I hope the above reply is helpful. Please do not hesitate to contact me directly if I can provide further information.
Kind regards,
Sarah
]
Sent: 01 December 2011 18:41
To: MHRA Central Enquiry Point
Subject: Seroxat
Dear Sirs
Seroxat
In 2002 I suffered a huge shock of attempted suicide six weeks after coming off Seroxat.
I have recently read an SSRi learning module for gps and am wondering why it took so long for me to be acknowledged as a victim of this prescription drug ‘severe drug reaction’ and suicide.
Nobody told me I would have an ‘adverse drug reaction’ to Seroxat, and it would help me greatly if you would tell my doctor that this is what happened to me.
You have written an illuminating guide to SSRI discontinuation symptoms and it would be great if you would let my practice know that you have discovered that ssri’s can cause self harm and potential suicide in a few patients.
AB
I agree with David,
The truth is being buried.
However, the internet has somewhat leveled the playing field in terms of giving voice, perspectives, and opinions of the patients and sufferers of side effects, medication induced damage etc . They cannot ignore the dissent happening on the internet, they are trying to but our dissenting voices are getting louder, and growing by the day. David’s analogy with the Catholic church is a good comparison, however most of the Church’s abuses happened before the internet age, often decades before the turn of the 20th into the 21st century. The difference not is that they cannot hide their crimes. The truth is there for all to see.
Well, well…
http://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(15)00166-2/fulltext?elsca1=etoc&elsca2=email&elsca3=2215-0366_201506_2_6_&elsca4=Forensic%20and%20Legal%20Medicine%7CLancet%7CNeuropsychiatry%7CPsychiatry%2FAddiction%20Medicine
There may be an easy way to resolve this question – Goodwin et al take high doses of their own medicine for 6 months, and see how it leaves them…after all, they are always banging on about how ‘safe’ SSRIs are – what could possibly go wrong?
Walter
Oh Mr. Walter K, if you only knew how many times I’ve dreamt of such scenario. Perhaps even have a Group on a high dose of SSRI for a year or two and then, unknowingly to the professor/patient, switching them to placebo?
After 5-7 Days of Cold turkey we’d start seeing some “characteristic pharmacology professor behaviour”…
We’d see “suicide by petri-dish”
(suicide note would be ghostwritten of course)
Professor runs perpetual motion with electrical discharge from own brain, calls invention “zapping Jenny”.
Professor seeks funding to find out wether it might be the actual placebo pills causing his reaction.
A public challenge by a prominent person or persons is in order.It doesn’t have to be a doctor; probably shouldn’t be. It could start with a hashtag on Twitter.
#OwnMeds?
I don’t see how anyone with an ounce of intelligence could say there is no link between antidepressants and violent behaviour in some people.
Pharma have pulled off the biggest scam of the century with antidepressant medications. The hype, the cover ups, the collusion and corruption. The casualties being buried in a sea of lies.
it isn’t that they cannot see the link is it Lisa, it’s just that they think that they are all-powerful and that the rest of us will forget, in time, all about their misdemeanor – will we? NOT LIKELY!! WE are the ones living with the fallout of their lies ( or our loved ones are).WE are the ones who keep being reminded of how things used to be. WE are the ones who have the flashbacks of the horrors they created.WE are the ones who wish we could wake up and find it was just a nightmare.WE are the ones who wish we could forget. THEY are the ones who can sleep at night feeling that they have done another good day’s work to swell the company coffers. So unfair isn’t it? I still feel that WE must keep our stories going, not just here but at every opportunity in the general public arena so that THEY may, eventually, be seen for what they are and what they really produce.
Well, well, well….Walter
http://1boringoldman.com/index.php/2015/05/27/a-study-worth-looking-into/#comments
As 1BOM extends his generosity to looking at Paxil Study 329, some of the drift wood has floated off, and, I, for one, was particularly interested in thoughts from Brett and Ryan who seem to be with us with inquiring minds………….and keeping up……
Annie, I wish that study was replicated instead. It was so manipulated that it must be virtually impossible to replicate.
GSK knows very well what they did or did not do, mostly Calling what they did
“research-techniques”.
I really like 1BOM, he seems more interested in actual facts than theories.
But I really dislike this “boomerang-effect”, that we Always turn our attention
to research that was false from the start.
The “yes-men” will deny the study being false. Or Point to other studies.
We know it was falsified and manipulated. Ghostwritten. Subjects were placed in certain Groups to make outcome look better. Data was read in the most generous way, and so on.
My idea comes from my slightly ‘rebellious’ mindset: I Think that GSK, when proven to wittingly falsify study 329, should recieve an automatic cancellation of all other Seroxat/Paxil studies. Because it shows them willing to falsify and cheat. Does it sound harsh? Well, it’s a pharmaceutical, we cannot have anything less than immaculate behaviour in such research field.
So what if you call me ‘ideaologist’ or ‘naive’. Certain things should be a certain way. It’s not up for discussion. And if they aren’t, we should change them in a hurry.
https://chrysmuirheadblogs.wordpress.com/2015/05/29/mental-health-patients-treated-like-animals-in-a-zoo-at-ablett-unit-in-north-wales-report-finds-itv-news-28-may-2015/
This is our local psychiatric unit – very well known to our family! Whilst I agree that the findings,if true, are disgraceful, I am not sure that we are being given the whole truth and nothing but the truth of this matter. I fear there might well be a hidden agenda – details of which I would rather keep to myself at present!
You are so right Mary. The trouble is though that a lot of people my son included feel ashamed by what happened to them. Rightly or wrongly they don’t feel able to share their story.
I will however never be able to turn away from what I have discovered over the past year. It’s been a terrible year and a journey I had no wish to take. It was definitely made easier by the support of some amazing people. Mary you have been such a help to me with your kindness, understanding and encouragement. I know that we will be friends for life now through the bond that we share.
My gratitude is endless to the person who helped me when I was desperately trying to prove something I knew was true. Without his expert knowledge and thirst for the truth I don’t know what I would have done.
I will continue to raise awareness wherever I can, support rxisk and DH will have my support, respect and gratitude till the day I die.
Thank you for your kind words – realising that I have been able to help you, in some small way, somehow helps me to feel that the horror that we all went through all those years ago ( still as vivid in my mind as if it were last year) was not in vain. I find it infuriating though that, generally, we are no further ahead in making it widely known of these dangers – even our GPs seem oblivious to the truth. Like you, I have no wish to rid the world of these medications but I do sincerely wish that we could get the word out to all people that using them does carry with it the possibility of adverse reactions.Like you, I had no idea what could happen whilst taking or on withdrawal from these drugs – our experiences are 15 years apart but exactly the same.For your son and my son’s sakes we owe it to them to fight on – their greatest reward for all their suffering would be to be able to say that they were the last ones to suffer in this way and that their stories have helped to keep others safe into the future.
As for the person that you found in your hour of need – there must be a whole gang of us who cannot thank him enough for being there, so willing to give of his time and expertise without counting the cost.Considering that we are a mere 30 miles or so away from the Unit that he was connected with, I am astonished that neither GPs, psychiatrist nor Legal team had knowledge of the truth that was already being expressed so close to home.The least we can do is help in the fight to get the truth out there.
Amen to that Mary. I’m sticking with David Healy and the truth.
This is probably tangential to the discussion, but I would like to vent my anger at the multi billion dollar supplement industry, and countless “alternative” practitioners, for perpetuating the same bogus myths about mood and neurotransmitters as the drug industry and mainstream psychiatry. Less dangerous, perhaps, but my God the money people spend thinking 5-htp is going to cure their depression which is caused by a serotonin deficiency, or oral GABA is going to cure their anxiety which is caused by a GABA deficiency, etc. etc. And it’s not just on the fringes, it is countless people with MDs after their name, offering urine neurotransmitter testing, quizzes to see where your “deficiency” lies, and so on. Shameful.
Not tangential at all
DH
Here is one such “brain quiz” offered by an MD. He misspells serotonin as “serotonin.”
http://pathmed.com/pdf/brain_quiz.pdf
Brain Deficiency Quiz – Why Take It? Your unique brain chemistry (the
combination of the neurotransmitters acetylcholine, dopamine, GABA, and
serotonin) controls how you think, feel, and behave. These deficiencies are
the direct causes of many medical problems.
Knowing how to restore deficiencies or imbalances is the way to begin
regaining your health. The results of this quiz will show you which
neurotransmitters you are deficient in, and how to correct it using
supplements. By addressing your deficiencies you will be on the path to a
healthier, younger you.
I don’t know how this is ethical???
Totally agree, Peter. Having suffered/am still suffering severe adverse effects of prescribed anti-depressant medications (which the medical profession has denied could be the case, despite me knowing from my own physical experience the genesis of my nightmare and having recorded in quite specific detail), I am bombarded from supposedly well-meaning friends that I should try Omega 3 fish oil, valerian, tart cherry, the blood-type diet, acupuncture, 5HTP, B Vitamins, Floradix, …oh it’s endless and exhausting to explain that none of these work. No wonder the “alternative health” industry is raking in the profits when there seem to be so many supporters of it. I just wish they would go through what I’ve gone through, even a tiny bit, to gain some understanding of what it is like to have protracted legacy effects from anti-depressants and know that there is nothing that can help (not that I or my GP/PDoc know of anyway).
As my previous surgery did not learn from Seroxat and experiences, they are now offering a Depression Service.
The form is below but has not reproduced the tick boxes due to IT limitations….
Are they now cutting out Psychiatric intervention and doing it all themselves?
As they have their own pharmacy, how likely is it that filling in this form will lead to a prescription of, maybe, even, Seroxat?
I read somewhere that doctor’s think in patterns.
When a patient walks in their brain power puts the patient in a category.
Heart, lungs, diabetes, cancer, or, another person who needs a day out shopping, as my lady doctor, so nicely put it……not remotely reasoning that the lists of questions are the result of cold turkey and messing about with psychotropic drugs of which they have no knowledge….from, maybe, even, Seroxat…..
Is this tangential?
• Alcohol Questionnaire
• Asthma Review
• Depression Questionnaire
• Text Message Reminders
• Carers Direct
• Pregnancy Care Planner
• Practice Policies
• In Times of Bereavement
Contact Details
Name:
Date of Birth:
Address
Postcode
Home Phone
Questionnaire
Over the last two weeks, how often have you been bothered by any of the following problems? Not at all Several days More than half the days Nearly every day
Little interest or pleasure in doing things
Feeling down, depressed, or hopeless
Trouble falling or staying asleep, or sleeping too much
Feeling tired or having little energy
Poor appetite or overeating
Feeling bad about yourself, or that you are a failure or have let yourself or your family down
Trouble concentrating on things, such as reading the newspaper or watching television
Moving or speaking so slowly that other people could have noticed. Or the opposite—being so fidgety or restless that you have been moving around a lot more than usual
Thoughts that you would be better off dead, or of hurting yourself in some way
Finally
Not difficult at all Somewhat difficult Very difficult Extremely difficult
If you checked off any problems, how difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?
About This Form
Fields marked with a red asterisk are
compulsory.
Thank you for agreeing to complete this questionnaire. Please fill in all of the appropriate fields and click ‘Send’.
A red asterix indicates a compulsory field.
Note:
By using this form you will be sending information about yourself across the Internet. Whilst every effort is made to keep this information secure, you should be aware that we cannot offer any guarantees of absolute privacy. If this matter concerns you then you should use another method to notify us of your information.
Personal Information
Personal information retained on this system is stored in a secure data centre located in the UK and is treated as confidential.
Have I misunderstood or is this a form that you fill and submit without even seeing a GP or Practice Nurse? Surely not! – more can be gathered about the state of mind of anyone by seeing their body language and tone of voice etc. than by the answer to a range of questions. I have often noticed that many of these sort of questions ( which you can find online to tell you if you’re suffering from this or that) give a choice of extremes in their answer choices – i.e. hyperactive/lethargic; sleep too much/ can’t stay asleep etc. which means that there is a very thin tightrope that we must walk along if we want to consider ourselves healthy! Maybe they would like to go one step further and make it into a Bingo game where the prize would be a prescription of your choice!
I studied the body language and tone of voice as they hurled insults at me.
You are not wrong, Mary.
Diagnosis by internet is creeping along. Pick up your pills at the Cash and Carry.
I don’t know what planet this particular Doctor is on. He thinks he is so smart.
He has already dropped himself in it by a neurotic telephone call to me from Prince Edward Island receiving my complaint whilst Islanders rejected him and his Medical Model.
As he returned with his tail between his legs, dragging his family through upheaval and financial crisis, he mentioned on his blog (nothing is secret on the internet) (ha), that his purchase of his Scottish Surgery was a ‘lifeboat’.
Interesting phrase…always keep your options open..I am almost certain that he is walking straight into another Seroxat disaster…these people always do..you just have to be ‘patient’ and keep your eye on your target…………….if you go around screwing up peoples lives, like him, I think it is a reasonable projection that he will do it again……….
BIN-GO:)
Dr. Healy,
Re:”Patients are still told in official leaflets for Citalopram their troubles are due to low serotonin.”
The level of neurobabble of escitalopram: doctors are also still told that the depressive symptoms of their patients are explained by low levels of serotonin in the synaptic cleft. It is stated that escitalopram decrease the symptoms of depression by “increasing the levels of serotonin and the activation of their neural pathways”
Here is the long version of the blog post (includes the excerpt of the official leaflet in Spanish): http://wp.me/p4UVo9-1xd)
Kind regards,
Jorge R.