This post by Peter Selley details yet another Selley triumph. It's extraordinary what focus and persistence can achieve. I am dedicating this post to Nikki Rutman, twenty years an analyst with the FBI, who currently heads up Moderna’s Global Intelligence Division. Moderna’s shares have plummeted since its 2021 Covid heyday. This appears unrelated to my FOI request which … [Read more...] about Secret Moderna Trial Documents
Safety or System?
Samizdat has just been graced with Gene Larkin's Seeking Soteria accompanied by Bill James fabulous artwork (graced is the best word). For reasons that will become clear, the title of this post picks up on the last post Unsafe Safety. Gene can be heard talking about Soteria with colleagues on a Mad in America Soteria Webinar. In the near future Katinka Newman will be hosting … [Read more...] about Safety or System?
Unsafe Safety
On March 20th, Senators Tina Smith and Ben Lujan, and Representatives Andrea Salinas and Becca Balint, sent a letter to the Secretary of the US Department of Health and Human Services, Robert F Kennedy, expressing concern about his promotion of disproven and outright false theories about mental health medications. In separate comments, Senator Smith indicated she had been … [Read more...] about Unsafe Safety
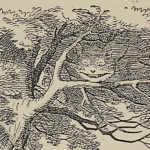
Six Weeks to Recover a Grin
I am among those who can be blamed for the disastrous MHRA supported drug label and messaging for antidepressants, along with Guideline recommendations that tell doctors and patients that it can take 6 weeks for antidepressant induced recovery to take place. This idea has been interpreted by MHRA and lots of psychiatrists and family doctors, who have no background in … [Read more...] about Six Weeks to Recover a Grin
An Appleby a Day Keeps the Doctor Away
Tangled up in Bureaucracy flagged a Signal for the Goose Signal for the Gander as a sequel. That was before the Gary Bullivant comments on Tangled up in Bureaucracy. If you don't normally read comments on post, the Bullivant-Kingston comments are in this link; they are worth reading. GB's comments fit nicely in with a delicious 2019 correspondence between Dee Doherty and Louis … [Read more...] about An Appleby a Day Keeps the Doctor Away
Tangled up in Bureaucracy
In response to Thomas Kingston’s death, Katy Skerrett, the coroner at his inquest, wrote to the MHRA (Britain’s medicines regulator) and to NICE (Britain’s guideline body) suggesting that their communications around antidepressant hazards appeared to downplay the risks of suicidal reactions to SSRI antidepressants, perhaps contributing to his death. See Aunts, Ants and … [Read more...] about Tangled up in Bureaucracy
The Respiratory Syncytial Virus Challenge
This post by Peter Selley centres on a Moderna RSV vaccine trial, the Rhyme trial, in young babies that was stopped last year when 7 out of 40 babies between 5 and 8 months of age developed severe lung disease, compared to 1 in 20 controls. Moderna had good reason to think its vaccine could cause this, as you will see, but the company appears to have opted to overlook the … [Read more...] about The Respiratory Syncytial Virus Challenge
Antidepressants Alcohol and Anne-Marie
Among the greatest triumphs linked to RxISK was Anne-Marie Kelly's discovery that SSRI antidepressants can cause alcohol misuse. A Hero Anne-Marie's story was first told in Out of My Mind Driven to Drink, which featured here in March 2012. This led to a post on RxISK Driven to Drink. Between them the posts have over 450 comments, a huge proportion of which say this describes … [Read more...] about Antidepressants Alcohol and Anne-Marie
Kingston’s Rule
This post is written by Dr Pedro who is watching events unfold from 10,000 miles away - with some extras added at the end. The UK Royal College of General Practitioners (RCGP) has been asked by Katy Skerrett, Senior Coroner for Gloucestershire, to respond to her Regulation 28 report to Prevent Future Deaths, after the inquest of Thomas Kingston (above). His death seemed to … [Read more...] about Kingston’s Rule
A Turning Point in History
That time of year thou mayst in me behold When yellow leaves, or none, or few do hang Upon those boughs which shake against the cold Bare ruined choirs where late the sweet birds sang. Shakespeare Sonnet 73 These lines came to mind recently when walking by a school playground crowded with young children on lunch-break. Like birds chirping in a tree or bush, they were … [Read more...] about A Turning Point in History