
More than any other group of drugs in medicine, the anticholinergics have become Maleficent – blamed for the hedge of thorns that keeps our inner beauty asleep until some medical prince can fight his way through and put a Magic Wafer on our lips.- See Experts by Experience.
In 1920 Otto Loewi had a dream that changed our world. Most people thought communication between nerves was electrical. Loewi suspected it was chemical. In his dream, he saw two beating frog’s hearts. Put in the right medium, hearts conveniently keep beating after removal from bodies. One heart had the Vagus Nerve still attached to it, the other didn’t.
The Vagus, or wandering nerve, is one of our main sensory systems. It wanders all over our insides connecting with uterus, bladder, gut, heart, lungs and feeds what is happening in them to our brain. These inputs are more than messages; they can enhance our mood, relieve anxiety, and even stop epileptic fits.
The Vagus also has a motor component, which through the parasympathetic system influences all our internal organs and when stimulated can slow the heart.
Loewi dreamt of stimulating a frog’s Vagus, and isolating the fluid where the nerve met the heart. What would happen when this fluid was perfused onto the heart whose Vagus nerve was removed? The second heart slowed. This demonstrated that neurotransmission was chemical, not electrical. The Vagus liberates acetylcholine which slows the heart. You can see the experiment happening Here.
Scientific breakthroughs that stem from dreams always sound romantic. Loewi wasn’t a typical researcher. He wanted to be an artist but was steered into a solid profession, medicine, by his family. Among his views of science, one deserves citing – a drug is a substance which injected into a rabbit produces a scientific paper.
Acetylcholine was the first neurotransmitter. It transformed atropine and other medicines, which blocked its effects, into anticholinergic drugs. These were among the most useful medicines we had around 1920. It enabled us to recognize histamine was a neurotransmitter and other useful drugs were antihistamines. Drug development was turbocharged. Antihistamine pharmacology gave rise to antidepressants, antipsychotics, antacids and others. We discovered noradrenaline, dopamine, and serotonin were neurotransmitters in the brain, balanced in systems containing acetylcholine ‘on the other side’. Anticholinergic drugs often relieved the side effects of their opposites.
Loewi got a Nobel Prize for his acetylcholine work, followed 34 years later by Axelrod for noradrenaline research and 30 years after that by Arvid Carlsson. In the 1950s, when Carlsson entered the field, it was still received wisdom that, whatever about the periphery, the brain operated electrically rather than through chemical neurotransmission.
Right up to 1961, when Loewi died, anyone surveying neuroscience would have picked out acetylcholine as by far the most important neurotransmitter and the anticholinergic drugs as among our most useful. But there were some new kids on the block.
The Only Good Anticholinergic is a Dead One
As outlined in Experts by Evidence, the 1965 catecholamine hypothesis created the original chemical imbalance in depression soundbite – a noradrenaline imbalance. Pure noradrenaline reuptake inhibitors, eliminating all other actions the early antidepressants had, like their anticholinergic effects, became the road to more effective and side effect free antidepressants.
The anticholinergic effects of the early antidepressants, which in terms of depression include a useful euphoriant effect, and which normally might be expected to compensate for problems caused by actions on noradrenaline, serotonin, and dopamine systems, became instead the cause of all side effects – dry mouth, constipation, blurred vision, withdrawal effects, neurological problems like tardive dyskinesia, and urinary retention. Soon afterwards confusion, memory problems, and dementia were added to the horrors of urinary retention.
Urinary retention featured hand in hand with dementia in an extraordinary 2022 article about overactive bladders which close to said one dose of Oxybutinin, then a best-selling anticholinergic bladder stabilizer, could cause dementia – See the Past Present and Future article below. The reason this ludicrous claim had some traction was that it came against a widespread belief that an anticholinergic drug could do just this – cause dementia.
Where this belief, at odds with what doctors could see in their patients, came from gives a key insight on modern pharmacology.
The background here is that the 1960s zeitgeist was that many mental disorders would, like phenylketonuria and Parkinson’s disease, be single protein or single neurotransmitter disorders. Depression was fingered as a noradrenaline disorder. Schizophrenia as a dopamine disorder. Anxiety a serotonin disorder. Dementia was the only niche left for acetylcholine.
Some 1970s experiments giving scopolamine, an anticholinergic, and demonstrating memory effects in volunteers gave some plausibility to this. The memory effects were not as dramatic as the problems following a low dose of a benzodiazepine or haloperidol. But they were enough to trigger a pharmaceutical industry quest for cholinomimetic drugs – anti-anti-cholinergic drugs.
Alzheimer’s was the noble, but only notional, rationale for this quest. The real goal was age associated memory impairment (AAMI). A lot of work went into making AAMI a recognized illness so that all of us over 50 could be persuaded that we didn’t need to have the little glitches we had begun to notice. We could all have the memory of a 15 year old, just as bisphosphonates could give us the bones of a 15 year old and Viagra the blood flow of a 15 year old.
A rake of cholinomimetics came on the market from the early 1990s onwards, but none did anything for dementia or AAMI. An offshoot of all this, however, was a Smart Drug market, with many Americans in particular buying into the idea of fine-tuning their cognitive states with chemicals.
All the while, little heed was paid to the profound episodic memory problems triggered by benzodiazepines. Many claimed they could remember little of the children’s childhood.
People complained of memory wipe-out after ECT. These problems were real but for the most part likely stemmed from the benzodiazepines and antipsychotics they were being tanked up on rather than ECT.
In 1991 the Beers list appeared. This was aimed at managing medication burdens in the elderly. Anticholinergics were the one group of drugs the elderly were definitely not supposed to be on, according to Beers. The Beers List had several iterations and copycat lists as deprescribing gained momentum. These lists universally recommended getting off anticholinergics.
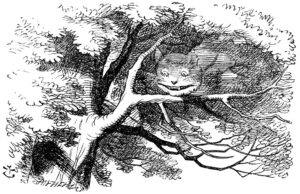
The Grin of the Cholinergic Cat
People who draw up deprescribing recommendations in general have even less links to pharma companies than bioethicists. But like bioethicists they are trapped by a ghostwritten literature and marketing copy.
As with the serotonin hypothesis of depression, which only emerged in the marketing department of SmithKline Beecham in the early 1990s, endless repetition can create as Jerome Gaub, speaking on theories about how the mind relates to the body, wrote in 1767
a “fable whose novelty has recommended it, whose recommendation has spread it, whose spread has polished it, refined, and adorned it with.. a pleasing look of truth”.
These fables or memes are an infection we contract from a ghostwritten literature – an infection these articles are designed to give us. Rather than hundreds of different academic authors writing the articles reporting the results of company trials, trying hard to get the science right, there are only a comparatively few bright women, along with the occasional man, who do the writing on all articles.
They do a good job from the material given them and slip in key and simple commercial soundbites like the known deficits of serotonin in depression and the known hazards of anticholinergic drugs. This rather than evidence is what cements in place the idea there is something wrong with the serotonin system in depression. And the idea that anticholinergic drugs cause problems.
In this way bioethicists coming to the literature on antidepressants in pregnancy figure it must be fine to give them to pregnant women and people like Healy, Mangin or Mintzes who quibble about this, flying in the face of a scientific literature should be struck off – See Risky Business.
Bioethicists are now major promoters of running company trials of drugs and vaccines in pregnant women – see Women, Pregnancy and Clinical Trials. and Not The BMJ News. What better cover for a marketing operation could a pharmaceutical company want.
The folk promoting deprescribing similarly face a literature which close to universally claims that anticholinergic drugs cause dementia. They take it at face value without going back to see if the claims are underpinned by substantial evidence. They aren’t. The 2022 review noted above refers to the claim that oxybutynin causes dementia from a study in which it seems one woman after a brief exposure became confused. Confusion and dementia are two different things. And one dose of an antipsychotic or a steroid or many other drugs can produce life-threatening confusion. But cases like these have little traction unless we already ‘know’ these drugs cause dementia.
The blindness runs deep. A recent FDA review blames the dizziness and confusion citalopram causes on their anticholinergic effects. How FDA reviewers can make this claim given the clear confusion and dizziness SSRIs regularly cause and the lack of confusion full blown anticholinergics is beyond me. But similarly deprescribing protocols lay the blame for dizziness and confusion in people on benzodiazepines or antihistamines on their anticholinergic effects.
What’s going on. The situation is rather like the James Holmes case, or any homicides triggered by an SSRI The evidence that the drug played a key part may be compelling but for a jury to acquit Holmes they have to accept that most of the medical literature on these drugs in the very best journals is ghostwritten and FDA are complicit in this. What jury, or bioethicist or deprescriber is going to do this?
Unless you were awake reading the 2022 review noted above, you might have missed the fact that it seems aimed at displacing oxybutynin in favour of mirabegron – a drug that Australian, German, Japanese and French authorities have cast serious doubts on owing to the risks of tachycardia, atrial fibrillation, hypertension and stroke it poses.
We can talk about the role of conflict of interest here as Barbara Mintzes and colleagues do in an article about the promotion of overactive bladder disorder, and bioethicists in general do, but the bigger problem is the fewer the links critics have to pharma, the less likely they are to realize that complaints about conflicts of interest suit pharma very well – they distract from the fact that the real problem is the ghostwritten literature and there is no substance behind many of the most iconic soundbites.
When the Old Guys Die
It used to be the case that scientific ideas rose and fell as the old guys died off.
But the force behind a lot of what pass for scientific ideas these days is much more a case of how many livelihoods the idea supports. If an idea supports a lot of livelihoods it persists. The chemical imbalance idea doesn’t just support the livelihoods of doctors – tons of people in the alternate health domain market their foods or vitamins for the effects they have on serotonin – see So Long and Thanks for all the Serotonin.
The idea that used to support medical livelihoods was that all drugs are poisons and it takes medical training to bring good out of their use.
Anticholinergic drugs are poisons like everything else but on balance they are now looking a lot less poisonous than SSRIs and many other psychotropic drugs in widespread use. Even nicotine, a cholinergic drug is looking a better bet that SSRIs for many nervous conditions, if taken in a safer delivery system than a cigarette.
The science, as opposed to the marketing, now indicates anticholinergic drugs and muscarinic antagonists have neuro-regenerative effects. Over a decade ago, Merck pulled benztropine off many markets because a Scripps Institute study had found that in a low dose it promoted remyelination. Merck’s hope, it seems, was that this was happening through some novel action, which they could optimize and patent and make a fortune – See Nobel Prize and Jackpot Winner. But it now looks more likely to be benztropine’s anticholinergic action.
WinSanTor have just reported another piece of anticholinergic magic – pirenzepine stimulation of peripheral nerve regrowth – both small and large fibres – in people with diabetic neuropathy.
If scientific ideas hinge on the livelihoods they support, the larger story for doctors is this. If deprescribing is the way forward, there will never be any RCTs or guidelines that help with this. Getting it right will need relationship based medicine, continuity of care, and a recognition of the hazards all drugs can cause – See What Counts. Doctors need to embrace a conflict of interest – for them to survive medicines need to be dangerous and it needs expertise to get people who are on 3 or more off them.
Knowing about the hazards means going by the science not by marketing copy. Recognising from the patients in front of them, or perhaps from their own experience of meds, that potent anticholinergics are less likely to cause urinary retention that noradrenaline reuptake inhibitors – See Experts by Experience and do not cause dementia.
Why might oxybutynin help women with bladder problems? Well SSRIs and other drugs can cause Interstitial Cystitis, along with prostatis for men – See Experts by Experience. These are likely neuropathies and oxybutynin, if its like other anticholinergics, may be helping restore the damaged nerve endings causing the problem.
It might be a deprescribing mistake to eliminate the one group of drugs that has otherwise been helping people tolerate the problems so many of the other drugs they are on have been causing.
There is a sister article to this one on RxISK – Experts by Experience. The academic version of both these posts is The Past Present and Future of Anticholinergic Drugs.


The Marketing of Anticholinergic Maleficence…
“accurately reflects the honestly held views of the clinical investigator authors.”
there is no substance behind many of the most iconic soundbites.
If an idea supports a lot of livelihoods it persists.
Putting GlaxoSmithKline to the test over paroxetine
Blockbuster antidepressant paroxetine is no stranger to headlines. The drug is now back centre stage as requests for clinical data from one of its trials are testing its manufacturer’s commitment to full transparency.
Peter Doshi reports
https://www.bmj.com/bmj/section-pdf/749788?path=/bmj/347/7933/Feature.full.pdf
Irony of study 329
There is a certain irony in the story of study 329 and its 2001 publication in JAACAP . In a letter to Jureidini, GSK explained that the JAACAP publication “was subjected to peer review on three occasions” and “accurately reflects the honestly held views of the clinical investigator authors.” But a more pertinent question is whether the published article accurately reflects the trial. In their most recent letter to GSK, Jureidini and his colleagues reiterate their need for the study 329 case report forms and their intention to analyse study 329 “following the original analytic plan.” As such, Jureidini’s team’s efforts to independently analyse and publish the results of study 329 can be viewed as perhaps the most “responsible” of all analyses—and one that it seems may yet overturn the JAACAP publication that GSK continues to defend.
“the hedge of thorns that keeps our inner beauty asleep until some medical prince can fight his way through and put a Magic Wafer on our lips”
10 October 2013 Andrew Witty tells US Fox News: “We’re going to publish all the data for all the trials that have been done since the company was formed”
As with the serotonin hypothesis of depression, which only emerged in the marketing department of SmithKline Beecham in the early 1990s, endless repetition can create as Jerome Gaub, speaking on theories about how the mind relates to the body, wrote in 1767
a “fable whose novelty has recommended it, whose recommendation has spread it, whose spread has polished it, refined, and adorned it with.. a pleasing look of truth”.
These fables or memes are an infection we contract from a ghostwritten literature –
You have to delve into pre-history to find and understand reported adverse events in trials of anticholinergics.
Probably most popular was Oxybutynin for overactive bladder – a poorly understood but much diagnosed condition probably linked with fibromyalgia and “interstitial cystitis”.
Back in 2009 a review by the Canadian Health Technology Inquiry Service came up with the same conclusion as Prof Healy – Cognitive Adverse Events are in the mind of the prescriber.
https://www.cadth.ca/sites/default/files/pdf/Oxybutynin,_Tolterodine,_and_Darifenacin_final.pdf