Editorial Note: Many people have wonderful responses to Humira and other biologic drugs like Enbrel (Phil Mickelson in the case of Enbrel). Rheumatoid Arthritis, Crohn’s Disease and the other conditions these drugs were first used for are debilitating disorders that need a potent treatment. But if a drug is potent it will have the capacity to cause significant harms.
Lots of people take part in clinical trials of new drugs believing they are helping to map out these risks for their families, friends, and communities. Doing so in the 1950s and 1960s when we had access to clinical trial data did a huge amount to save lives especially the lives of our children and to free us from disability. No longer.
Those who are injured by new drugs in trials end up unwittingly further injuring their families, friends and communities when their data is hidden – because companies like AbbVie then go on to claim that the science does not support a case that their drug can cause harms.
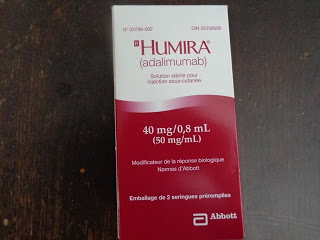
Annette McKinnon (@anetto) got in touch with us after reading some of the recent posts about Humira – saying that we were not letting people know how helpful Humira can be. We agree and invited her to paint the positive picture – what happens when the drug works well. This she has done here.
Annette’s Story
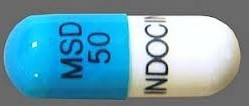
When I first developed RA the treatment plan given by my Family Doctor was to take a maximum dose of aspirin (12 pills a day) for a three months to see if that would have a beneficial effect. Over those months damage continued to occur. Since this treatment did not seem to make a difference I found another doctor. His treatment was NSAIDs, specifically Indomethacin: That resulted in gastro problems added to the pain, swollen joints, weight loss and fatigue.
When I finally saw a specialist over a year later he outlined the possibilities The most aggressive treatment in his Pyramid of Possibilities was immune suppressant drugs. I was prescribed gold injections and then transitioned to methotrexate. Over the years the methotrexate was combined with almost every other DMARD (disease modifying anti rheumatic drug) possible. I kept trying all the combinations hopefully over the years until I became more involved and informed about treatments and possible choices. Once I was aware that methotrexate does not actually stop damage to the joints and found out there were other choices that did stop joint damage I campaigned for treatment with a biologic drug.
In my reading I had learned that biologics produced a greater sense of well-being and a better quality of life at the same time as they stopped progression of damage. I saw the info above in online CME (Continuing Medical Education) courses during the time that pharmaceutical companies were the major sponsors of many of them. Reports of drug trials like the PREMIER Study and ARMADA were a further influence on my desire for biologics.
I combined this knowledge with the facts of my life. I was working full time but all other areas of my life were neglected because of pain and fatigue. Most of the time I was not at work was spent resting up to be able to continue to work. My exercise tolerance was very poor. It used to take me two days to recover from any efforts beyond isometrics. Now with Humira my recovery time from exercise seems normal and I am able to do more in a day than just work.
There has been great progress in the treatment of RA over the past years. Prior to 15 years ago there were only 7 new treatments found in 70 years. Now it is hard to keep track of all the new alternatives. The improvement in treatment is noticeable even by the look of the people waiting at the rheumatology clinic. No wheelchairs and very little visible damage can be seen now.

Progression is the major factor in my choice. I can’t afford to have any new joint damage. While only one active joint may sound like good control to many, when that one joint fuses it’s useless for good and the disease moves on to another one. There are no miracles in RA that unwind joint damage.Over the past 7 years that I have been taking Humira I have been sick 4 to 5 times with colds and flu and the severity has seemed worse but not the frequency.
I have been influenced by this great talk by Dr Edward Keystone called The Most Exciting Time Ever In The History of Arthritis and by Dr Shashank Akerkar’s blog post called Time, tide and inflammation waits for nobody.
The choice of Humira as my biologic was mine. The Dr I was seeing gave me a choice of the 3 major anti-TNFs. I had concerns about one and chose Humira based on the ease of use and my schedule.
Despite my enthusiasm for effective treatment I am anxious to see full disclosure of significant risks through the release of data from clinical trials. The legal action blocking disclosure of trial data by pharma companies Abbvie and InterMune is a step backwards for patient safety. There is a petition here against the lawsuit. Their lawsuit has shut down the whole public access program of the European Medicines Agency. Patient safety is not a trade secret! To paraphrase @ePatientDave “Give us our damn data.” If we are choosing to take these budget busting drugs we should have access to data about them.
Annette, thanks for writing this – and I hope the treatment continues to work for you!
I agree with you and E-Patient Dave: “Give us the damn data!” And I’d add a comment from Sean Ahrens, who founded the online community Crohnology: “The Right Stuff Isn’t Being Studied.” The best approach to auto-immune diseases would be to find out what’s provoking people’s immune systems to flare up and start attacking their own tissues in the first place. Unfortunately, that wouldn’t lead to the development of profitable products … so that’s not where the research dollars go.
Producing medicines that suppress the immune system is a much riskier strategy—it’s like fiddling with the brakes on your car. It might cost you a couple of minor fender-benders, or it just might cost you your life. It may be the best option right now for people with severe rheumatoid arthritis. If so, the right to know is at least as important for those who take Humira as for those who might decide it’s not worth the risk. Many of the most serious risks could be made more manageable, if only patients knew what to look for. That’s certainly true with skin cancer, which can often be treated easily if caught early but be life-threatening if it’s not. The same is true of some lung infections like histoplasmosis.
In that way it reminds me very much of the antidepressant situation. How many of those who committed suicide would be with us today if they’d just been given a simple warning: “Listen, there’s a good chance this drug will make you feel better … but there’s a small chance it might make you very nervous and upset, or give you strange thoughts. If that happens, call the doctor right away – and be aware that it’s not you, it’s the drug.” There is no excuse for the failure to warn.
Even though the dangers of antidepressants particularly SSRIs have now been outed there is still much denial by GPs and Pharma that it’s the drugs.