Editorial Note: This is part three in the Change in Chicago series covering the Dolin trial and its implications. Like part 1 it is written by Johanna Ryan – The Dolin Verdict and Playing Go.
By twenty-first century American standards, Stu Dolin’s medical care was close to ideal. That’s a hard idea to swallow, given what happened to him in the end, but it’s true. The real paradox is why it wasn’t enough to save him – and how his doctor became a victim as well.
In June 2010, while taking a generic version of the antidepressant Paxil, Dolin jumped in front of an oncoming subway train in downtown Chicago. His family was convinced that the medication had caused his suicide. Last month, a federal jury agreed. They found GlaxoSmithKline (GSK) liable for Dolin’s death, and awarded $3 million to his widow Wendy – two million for her own loss, and one million for Stu Dolin’s own suffering in his last week of life.
Few people succeed in suing the drug company when a loved one dies from the effects of his medication. It’s far more common to sue the prescribing doctor. Plenty of lawyers are willing to take on a malpractice insurer with limited loyalty to the doctor, and a lively interest in a reasonable settlement. To face off against a multinational corporation with an unlimited war chest, which will fight like hell for the reputation of its product, is something else entirely.
An even bigger barrier is something called the Learned Intermediary Doctrine. Under American law, drug companies have no obligation to level with you, the patient, about the potential hazards of the drug. Their only obligation is to tell your doctor about those risks. He or she is then expected to function as a “learned intermediary” – a sort of educated bodyguard who will tell you what you need to know, in language you can understand, and see to it that no harm comes to you. The drug’s official label (that enormous, technical document folded up and stuffed into the drug package) is written with your doctor, not you, in mind.
But what if that official label does not tell the whole truth about the drug’s hazards? That was the situation faced by Martin Sachman, M.D., Stu Dolin’s family doctor, who became a key witness in the Dolin lawsuit.
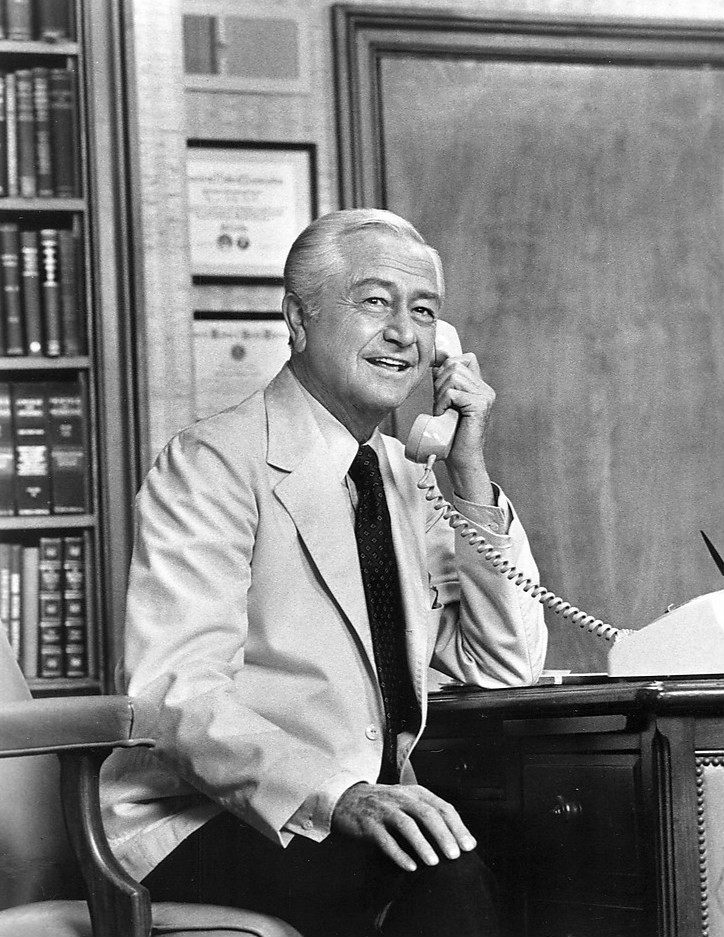
Marcus Welby M.D. – the old-school family doctor
That’s not Martin Sachman in the picture at the top of today’s blog – it’s Robert Young in the title role of Marcus Welby, M.D., the popular prime-time TV drama from the 1970’s. To most of us, Dr. Welby represents the family doctor we wish we could have – the one our parents had in the good old days. He was a settled presence in the neighborhood; he’d known you and your family for years. You could go to him for advice on just about anything, and you tended to trust what he told you.
For Dolin, Marty Sachman was that kind of doctor. Since about 2005, Sachman has had what’s known as a “concierge” practice. For an annual fee of about $2,000 (over and above their usual insurance costs), patients can get something close to a Marcus Welby level of care from a doctor of this type. They can be reached on weekends, may even make house calls from time to time, and you’re almost never limited to a ten-minute appointment.
Sachman had been Stu Dolin’s doctor for at least ten years. He was also a close personal friend. (That’s unusual enough these days that attorneys rushed to assure the jury there was nothing “unethical” about it. A generation or two ago it was fairly common, especially in small towns.) Often, faced with a difficult medical decision, there’s one question we really want to ask the doctor: Would you give the same advice to a loved one or a best friend, if they were in my shoes? Mostly, we don’t have the nerve to ask. Stu Dolin was lucky enough to know the answer would be yes.
A Job For A General Practitioner
Most family doctors take that Learned Intermediary business fairly seriously. It’s one reason why they refrain from handling “specialty” drugs for complex or serious conditions, which may require expert management. Chemotherapy for cancer; biologic drugs for Crohn’s disease, MS and other autoimmune disorders – those are best left to specialists.
When he began practicing medicine in the 1980’s, Sachman explained, antidepressants were in that category. The older ones were more problematic, with more side effects, and were reserved for people with relatively severe symptoms. Rather than try to treat such patients himself, he’d refer them to a psychiatrist.
This changed when Paxil, Prozac and the other SSRI drugs came out in the early 1990’s. They were depicted as being safe enough to be handled by general practitioners, and a reasonable option for patients whose troubles didn’t warrant seeing a psychiatrist. By the mid-2000’s, this had become the first-line option for dealing with both depression and anxiety.
As Dr. Sachman saw it, if a patient had mild to moderate depression in response to some trouble or stress in his life that was a “reactive” depression for which he could prescribe SSRI’s. If they had serious problems with sleep and appetite, a slowed-down or unusually agitated appearance, and an inability to function in daily life, that was true “clinical depression,” and they should see a psychiatrist.
Dr. Sachman knew Stu Dolin well, and the anxiety he complained of in June 2010 did not alarm him. Stu was just going through “one of his stress periods, on account of his work responsibilities. He seemed to be getting through it like he did the other times.” Dr. Sachman’s diagnosis was situational anxiety. A drug like Paxil could help people get through a rough period like this. The condition was fairly benign—and like the overwhelming majority of his colleagues, he considered Paxil to be a fairly benign drug.
A “Warning Label” that failed to warn
By 2010, the official label for Paxil gave physicians no reason to doubt that assessment – at least for adult patients. It warned that any antidepressant could trigger agitation and suicidal impulses in children and youth up to the age of 24. However, it also stated that “short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24,” and showed lowered suicidality in those over 65.
The warning added two more crucial sentences:
“Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality or unusual changes in behavior.”
As psychiatrist Joseph Glenmullen told the jury, this label effectively blinded doctors to the risks faced by adults: “What this tells me as a practicing psychiatrist is that if I’m treating a 57-year-old patient, and I put them on Paxil, Paxil couldn’t make them worse. Paxil couldn’t make them suicidal.” If they did feel worse, said Glenmullen, “it would be, and it says explicitly, their depression or other underlying psychiatric condition.”
Worst of all, he said, “if the patient gets worse and it might be the drug, what do you do? You take them off the drug to see. If they get worse and it couldn’t be the drug but it’s the depression, what do you do? You increase the drug, which is going to worsen the risk. So it’s very dangerous.”
The regulatory history of Paxil and the other SSRI’s was almost Byzantine. For years they carried no warnings of a risk for suicide. In 2004, after thousands of troubling reports, a Black Box warning was finally issued for children and adolescents. A number of medical experts felt the warning should apply with equal urgency to adults.
However, in 2007, the FDA decided on a uniform warning for all antidepressants, old and new. This was the “24 and under” label attached to both brand-name and generic Paxil in 2010. This suited GSK just fine. The FDA invited the company to discuss whether additional warnings were needed for Paxil, but GSK never took them up on it.
More importantly, it never fully shared with the FDA—and still less with doctors in the community—what it knew about the real risks of its product. In fact, GSK had known since 1989 that its drug could trigger akathisia, an agonizing combination of physical restlessness and emotional turmoil that could lead to suicide. The risk applied to both teenagers and adults; at least twenty suicides had occurred in patients on Paxil in clinical trials, the majority of them in people over age thirty.
A Doctor Taken Hostage
Thanks to GSK, that information never reached Marty Sachman. If it had, he testified, he would never have prescribed Paxil for Stu Dolin. There were plenty of other options—other drugs, and non-drug strategies – for treating situational anxiety. Because of the warning label, he said, he had never prescribed Paxil to a patient under 25; the benefits didn’t seem worth the risk. He had a few adult patients who seemed to do well on Paxil; if they had been on it for several years and wanted to continue, he would refill it. However, in the seven years since Stu Dolin’s death he had not written a single new Paxil script: “I don’t trust the labeling,” he said. “I don’t trust the company, to be honest.”
Marty Sachman’s anguish—and his sense of betrayal—was apparent to everyone in the courtroom. Physicians like himself, he said, “rely on truth and honesty from pharmaceutical companies, and to falsify information or hold back information is totally criminal. How can we treat people effectively and safely if we can’t depend on that?” They couldn’t. Instead, he had prescribed a drug, and a patient had died. That alone would have been traumatic for any honest doctor; that the patient was his best friend made it devastating. It was not like being a Learned Intermediary; it was more like being a hostage.
So what about the average Joe?
Dr. Sachman never got the chance for a follow-up visit with Stu Dolin; within six days of starting Paxil, he was dead. If he had, it’s just possible he could have spotted his longtime patient’s real problem. Maybe even stopped the Paxil. We’ll never know.
In 2010, the year Stu Dolin died, doctors wrote 259 million antidepressant prescriptions. For most patients, who don’t have access to anyone remotely resembling Dr. Welby, the situation is even scarier. They may get a script for an SSRI in a ten-minute encounter with an overworked stranger, based on a checklist left in the waiting room so that every patient can be “screened” for depression. The potential number of doctors taken hostage – and patients tossed overboard – is hard to imagine.
I have to think genial old Marcus Welby, M.D. wouldn’t stand for it. What about us?
We had quite a ‘nice’ almost Marcus Welby-type GP in 2001. We’d known him a bit over the years. He was pleasant and conscientious and we felt lucky to have him. Ditto others in his Practice. But that feeling of safety and relaxed trust in the relationships ended abruptly when the wind changed ie after our son Olly had Seroxat prescribed for him.
As Olly changed and what was clearly AKATHISIA set in, this GP lectured us over the phone about being the cause of Olly’s problems because we’d listened to his concerns and believed him. We were over involved and over protective, it couldn’t be the drug, blow the PIL, it had to be us. Family on Olly’s dad’s side, and Olly’s brother and wife-to-be pitched in too, also rubbishing our concerns. (All families have issues – ours was that Olly was very much brighter than all the others, had achieved amazing academic results whilst remaining a delightful unassuming person, and there was a lot of silly jealousy flying around. One dares to suppose that they were rather pleased to see him floundering at last, the golden boy no longer glittering out front). Sad to say, once you manifest AKATHISIA and no one wants to connect it with Seroxat, you are stuffed.
It was the end of our son’s Uni career, and the end of our feeling of safety with our GPs. We went on, genuflecting to them in their superiority and trying to keep these tigers from swishing their tails but things were never the same. They never quite will be. Our son died, yes, but worse than the dying was the torment, leading up to it over the years, of not being correctly diagnosed, and not being believed. And still, I guess, certain family members will never really ‘get it’ because they are still brown nosing and genuflecting to their godlike doctors, having let their common sense fly away just because these medics are medics, or Marcus Welbys, who know best of course.
Thanks again, Johanna, for an interesting addition to your former points concerning the Dolin Trial. Has this trial and its result opened up conversations far and wide in your area I wonder? I find it so frustrating that, here in the UK, there hasn’t been any mention whatsoever in the news – neither TV/radio nor newspapers ( not to my knowledge anyway). Is this simply because of big business pressures leading to fear of reprisals or does it have more to do with a general apathy, leading to a decision of not bothering to share information which will only concern a section of society?
I had expected that the outcome – that GSK were responsible, or, if that didn’t stick, then it was the FDA that were at fault – would have been welcomed far and wide. At last, the prescriber was not being blamed and neither was the patient. It wasn’t the patient’s mental state that was at fault and neither was it life’s circumstances that created the downfall. No – it was the lack of information from the pharmaceutical company or it was the lack of information sharing. The blame was directed at the top – and there it stayed. A story worth sharing surely?
Upon reading the verdict, I got in touch with the niece of mine who is a statistician at Liverpool Uni., wondering what they made of this result. She had no idea that such a trial was in progress, never mind knowing the verdict! I couldn’t believe it. I really thought that it would have been of interest to such people – actually, she was really interested and went on to find out all about it – people who deal with medical stats. day in and day out to know what goes on in the pharma world, obviously, I was wrong!
I have to say, I’ve been quite encouraged that the case got as much press coverage as it did! Which was one round, for one day or so. To use it as a springboard for challenging people’s manufactured assumptions about SSRI’s will take a lot of time and effort.
Several people have told me, for instance, that they don’t see how this could have happened, as these drugs take three or four weeks to have any effect at all, at all. It’s one of those things “everybody knows” that just ain’t so — and probably convinces a lot of people who feel worse on SSRI’s that it’s their own illness at work.
One thing it taught me was to deepen my cynicism about “independent” “non-commercial” outlets like National Public Radio. Every other news outlet in town referred to the drug as PAXIL in their coverage. Only NPR, in its two-line throwaway coverage, called it “paroxetine.” Very sensitive … to SOMEBODY’s needs!
Glad it got some coverage anyway Johanna. Hope you’ve framed some of them for posterity – ready for the day when ALL believe what we know to be true. You can produce them, at that time, and proudly declare “I know ‘cos I was there”. As for the argument of can/can’t cause difficulties in the first few weeks of ingesting – it’s my belief that they can cause havoc within HOURS, never mind weeks, for some unfortunate individuals. Paroxetine – Paxil – Seroxat – whatever the name, each small tablet contains the same destructive element which destroys the lives of many users.
Everything that you say regarding GP issues are quite understandable, Heather, considering the consequences of his prescribing on your family. Having said that, maybe we do need to consider the GP’s situation in this – as seen at the Dolin trial, the GP was not given the whole truth regarding the akathisia/ suicide link, therefore he was not held responsible. My feeling, like yours, is that he jolly well SHOULD have known – but, not having ever walked in his shoes, I do feel that my feelings are probably a reaction to an experience rather than a considered opinion. Throughout his fifteen years since being given that prescription for Seroxat, Shane has remained adamant that his GP did what he considered to be BEST SUITED for Shane’s needs AT THAT TIME and won’t have any criticism of his GP’s decision. I accept that opinion but do feel that GPs should be better prepared for an adverse reaction should one manifest itself. There is, by now, enough information out there for every GP to be totally aware of the POSSIBILITY of a reaction; whether that is likely to happen very rarely or not should have no bearing whatsoever on their acquisition of the facts. They MUST take responsibility for each and every patient that they treat surely?
Dealing with Ro- Accutane is slightly different in some ways. Handing out prescriptions for antidepressants, in anyone’s book, is tricky. Handing out prescriptions for an acne cure – what can possibly go wrong? We know that the truth of the Ro Accutane story is far from simple. Where both the Seroxat and Ro-Accutane stories are so similar is that the possible complications ARE KNOWN and are being DISMISSED – it seems, since some patients must be sacrificed for the sanity of the others. So unfair. There again, aren’t we living in a ‘democracy’ where many are ‘sacrificed’ in everyday life for the ‘sanity’ of others? If only the issues of everyday UK life were changed, maybe then we would have a better chance of changing attitudes towards the realities of Seroxat, Ro-Accutane and all the other problematic products.
We amazingly seem to blindly accept ‘collateral damage’ – the deaths of some for the cure of others. Like with vaccines. But with Roaccutane, so MANY are dying, after lives filled with torment, and the traumatised parents are left in disbelief after each death. “We tried so hard” they protest, “but in the end, all in vain.”
As you say Mary, all they did was take a medically pushed-on them course of pills for acne. So some of us just cannot accept these collateral deaths any more. Some go on fighting (like us) but never seeing the wind change. Some curl up with a bottle of gin and hope it will all go away, and who can blame them? Some even end their own lives too. The system is corrupt and wrong. But who’s going to change it, and how?
Interesting ‘Details’ about the ‘Doctor’ in a Paroxetine Suicide ..
‘Dr. Breggin testified that the negligent prescription of the antidepressant Paxil (paroxetine) caused Mr. Mazella’s condition to deteriorate, ultimately causing or contributing to his suicide. In addition, Dr. Breggin testified that Dr. Beals abandoned the patient, further causing or contributing to the tragic outcome.’
Paxil Suicide Retrial Settled by Defendants
May 16, 2017
In 2014, psychiatrist Peter Breggin was the medical expert in a case involving a Paxil-induced suicide and helped the surviving family win the malpractice suit. The case was recently overturned on a technical issue and resumed last Monday, resulting in a settlement the following day.
Click here to read Dr. Breggin’s description of the case, report to the judge, and 37 accompanying scientific articles.
https://www.madinamerica.com/2017/05/paxil-suicide-retrial-settled-defendants/
What your doctor may not know …
http://breggin.com/joseph-mazella-vs-william-beals-md/
Would Stu Dolin have been any safer if he’d gotten his meds from a “specialist” in psychiatry, rather than a mere GP? I don’t think so.
It’s hard to say, of course. Only one professional helper had a chance to see him after he began taking Paxil – his counselor, Ms. Reed, the night before he died. He said he felt like he was having a nervous breakdown, and she was alarmed at how agitated he seemed. She called him the next morning to urge him to see Dr. Sachman, but it was too late.
If anyone could have “rescued” Stu, I think it would have been one of these two people who actually knew him well, and could recognize that this was different from his usual complaints. True, doctors and counselors across the board have been miseducated about the risks of these drugs – Marty Sachman would be the first to admit he had far too much confidence in their safety. Thanks to GSK.
But I think the average psychiatrist has more misplaced faith in SSRIs than any non-specialist. They would have been more likely to decide they had a serious mental illness on their hands, and raise the dose of Paxil in just the disastrous fashion predicted by Joseph Glenmullen. Or added a second drug to the mix. Psychiatrists feel more confident in doing these things than do non-specialists …
They also would have chided Marty Sachman for using out-of-date terms like “reactive depression” and “situational anxiety.” Psychiatrists seem to have abolished the distinction between distress that comes on in response to tough times in life, and a constitutional mental disorder. It’s all the same disease entity – and since this was Stu’s third or fourth spell of being “a bundle of nerves” in response to high-pressure work demands, they would have recommended lifetime medication for sure. Sigh.
Mary, I take your point about GPs, and I take Shane’s on board too. However, I think there is a current fashion for brushing aside the opinions of loving parents when they express concern about their offspring. Don’t let us be in any doubt, most parents love all their children deeply, and when they see them in distress, they’ll do all they can to help. It’s a natural response, but so often ‘tough-minded’ health care professionals castigate this caring attitude as overbearing and unacceptable. So they exclude them and turn their backs when concerned parents report adverse behaviour, observed as medication-induced, by their loved ones. This is SO terrifying for any loving parent with an ounce of empathy. The loved one, already struggling with worry about their condition and possibly in the grips of AKATHISIA, now hear that their parents are likely their problem (never the medication of course…) so they feel weak for having confided in them, and thus another anchor point has been kicked away. This is frankly madness. It causes terror in the parents, caught between a rock and a hard place. The parents end up almost as sick as the offspring.
So, if a GP can stop reverting to this idea of blaming the parents, like an automatic reflex response to every young person’s mental health unwellness, maybe the oiled wheels would begin to turn more smoothly and more youngsters would keep anchored to at least one certainty – that they are LOVED beyond all belief by those who brought them into this world, who gloried in the joy of seeing them growing up, and only ever want the best for them. So, GPs need to listen up and take notice of this, please.
Change in Chicago: Dr. W…… on the Witness Stand ..
“It summed up the attitude of many doctors to the condition that he made his speciality. But it also encapsulated a widespread belief about mental illness: it wasn’t real like physical illness. It did not involve cells and cancers, it dealt with chimeras.
“Neurologists used to say to me: ‘You seem like a nice enough chap, why are you doing psychiatry? None of your patients get better.’
That was rich coming from neurologists. But it was also not true. We have very good outcome rates. It was simply factually wrong.”
Now, as Professor Sir Simon Wessely, president of the Royal College of Psychiatrists, he is in a position to do something about it.
http://www.independent.co.uk/life-style/health-and-families/features/simon-wessely-if-we-treated-people-with-diabetes-the-way-we-treat-those-with-depression-there-would-9924174.html
Chi•me•ra
also Chi•mae•ra (kī-mîr′ə, kĭ-)
n.
1. Greek Mythology A fire-breathing female monster usually represented as a composite of a lion, goat, and serpent.
2. An imaginary monster made up of grotesquely disparate parts.
The W. Pickles Lecture
A new kind of doctor
http://gphealth.nhs.uk/wp-content/uploads/sites/37/2017/05/RCGP-William-Pickles-Lecture-A-new-kind-of-doctor..pdf
Simon Wessely Retweeted
Clare Gerada @ClareGerada May 19
My William Pickles lecture given last week to my profession http://gphealth.nhs.uk/wp-content/uploads/sites/37/2017/05/RCGP-William-Pickles-Lecture-A-new-kind-of-doctor..pdf …
Betrayed by the Doctors
SCANDAL BY NUMBERS
– 2-4 weeks is the maximum time that bonzodiazepines should be prescribed
– 250,000 UK people are prescribed the drugs for more than six months
– 6-18 months is the time is takes to see the effects of withdrawal symptoms
– 800,000 people have wrongly been prescribed ant-depressants long-term
Betrayed by the doctors who turned us into DRUG ADDICTS: How a nation of patients became hooked on prescription pills
Fiona French was given prescriptions for benzodiazepine drugs to treat epilepsy
The social scientist from Edinburgh sound herself on the medicine for 40 years
Here, she describes the struggle to come off them – and her fight with addiction
By John Naish for the Daily Mail
Published: 22:27, 22 May 2017 | Updated: 00:06, 23 May 2017
http://www.dailymail.co.uk/health/article-4531548/Betrayed-doctors-turned-DRUG-ADDICTS.html
Paul Flynn, a Labour MP and vice-chair of the All-Party Parliamentary Group for Drug Policy Reform, adds: ‘The history of politicians’ broken promises for action on these drugs is so bad it threatens to give cynical opportunism a bad name.’
I am not first to tell that SSRI ruined my life. The worst thing is permanent blunting of all possible emotions and personality. This started when after going cold turkey from 1 year long venlafaxine, I felt extremely emotional. Because fear of depression rebound I went to doctor and he prescribed escitalopram. After just few hours I felt significant blunting of emotions. It was bearable then. however, overnight, after second dose blunting was very brutal. I suddenly felt like my whole personality dissociated, lost emotional/mental drive and feeling of any emotions. My speech and ability to self-express became extremely poor. I just couldn’t feel any drive to make complicated sentences and even simple actions. I ceased all my activity, including communicating/meeting friends, watching movies, listening music, using computer, do sports and my hobbies ( DIY, Guitar, Motorcycle). I stopped caring about hygiene. I was just sitting on chair and staring at wall. After 1 one week my parents took me to neurological unit. Then I told all of them about what happened. The young doctor initially diagnosed me with frontal lobe syndrome and told me SSRI might be culprit because there are case reports in children/adolescent ( I was `19yo), but he wasn’t sure. Also sent me to take MRI. However, next day two older came in and they said that SSRI can’t do this and It’s something else. They moved me to psychiatric clinic. Then drugged me heavily. My speech became only “Yes or No” or other single words or nothing at all. They kept me in this state for two weeks and then lowered/changed meds. I returned to an earlier state, the same as first day in a unit. Two weeks after they discharged me and told that I have negative symptoms of schizophrenia. They also said I could have at some point psychosis but It went unnoticed
One year later I still have a symptoms. I am very disabled socially, have no ability to work/study and live only from social benefits. Also suffer from insomnia ( my ability to feel tiredness is somehow blunted) and lack of sexual desire. Doctors keep telling that what happened to me is schizophrenia but I don’t believe them.The feeling of emotional blunting is the same as when I was taking venlafaxine it differs only (extremely) in severity. In rare moments of improvements I want to kill myself because I can emotionally processes what happened to me.
Hope someone takes into consideration how looks like the worst possible outcome from medicating depression. This is the only place when I can speak about it, everywhere else my comments have been deleted by moderation or just downvoted
Markus, your history mimics mine. I’ve been over and over it a thousand times since I learned about the hidden truths of SSRI’s. There is no humanly possible way for the patient, you and me, to halt what happens. The very essence of being blunted by your pharmaceuticals prevents you from making rational sense of what is happening to you.
And I grew up as a very rational and cautious young man who was always trusted by my surroundings. Whatever the situation, it was unheard of for me to make a down right irresponsible decision.
But since my very first pill of SSRI I just “gave up”, nothing was important anymore.
Today, almost 20 years on and despite knowing what the drug does to me, I can’t stop it. I tried to taper, but at a quarter dose I got so overwhelmed by emotions that I saw no other way than to go back on higher doses.
I litteraly walk around with 20 years of bad decisions and “un-cried” tears bottled up inside me.
There is a whole lot of people facing problems like ours.
I have no advice to give, but educate yourself and read Healy’s blog for inspiration.
Ove, Sweden, 2017
Markus, thank you so much for describing so graphically how you feel, having been on Venlafaxine and later Escilatopram. It has made certain things much clearer to me and my husband.
Our son, in the last three years of his life, was on these two meds, one after another, but in the reverse order to you. And he tried to explain to us how he felt, but at some times he could hardly talk, in the sense that he said he couldn’t think or find words, and worst of all was the emotional blunting, the deadness in his heart, which was always there. He did have some outwardly happy times and put on a good act for his friends, but he told just us (and maybe a few others, I don’t know) how lost and confused he felt, and the worst thing was, he died believing that what he felt was his own fault, some personal mental weakness that he hadn’t managed to conquer. He really believed this. GPs and various psychiatrists who he had met fleetingly at different points in his life after he first began to suffer low mood (having been prescribed RoAccutane) all denied that medications like the acne drug and then Seroxat SSRI and then a cocktail of others in 2002/3, could do this. ‘It had to be his own psyche which needed effort on his part’ etc. And boy, did he put in effort. He never stopped trying to ‘sort himself out’ as he was made to feel he should. His worst blunting came in 2010/11 when the Escilatopram began. In the last 6 months he was alive, in 2012 he was taken off that and put on Venlafaxine. Then eventually told to stop that at once by a Home Treatment Team Lead psychiatrist ‘as he was not depressed’. By then he’d got OCD suicidal thoughts. On stopping, he had the most horrendous withdrawal symptoms and AKATHISIA, but was told by this same worm of a psychiatrist that if he didn’t effectively pull his socks up, he would carry on leading a life of crippling OCD and misery. But he gave him Olanzapine (for some reason, whilst telling him, well, and shaming him in front of us and the Home Treatment Team, that he was not suffering depression and his expressed wish to die was just attention-seeking behaviour! No one ever admitted in 11 years that it was the drugs they’d prescribed for him, not he. We could see at the beginning in 2001 that it was and tentatively dared to suggest that to the GP but were shot down in flames for being delusional and talking rubbish. Our brave son lost the regard of the rest of his immediate close family, except for us. He was isolated and felt rejected by them. They too probably didn’t accept it was the drugs that made him change into a withdrawn person. He did end his life, but how tragic that was and how awful, because we now know from people like you, what was REALLY happening to him, and we could have helped SO much more and challenged that worm psychiatrist with some authority and knowledge. Not a day passes that I don’t wish desperately that he had found this RxISK Blog and Dr Healy in time, and understood himself at last, with a great sigh of relief. Wherever he is now, he will of course realise all this, but too late for us to have the joy of his company here for the rest of our lives.
So Markus, thank you for what you have explained. He let those inept irresponsible doctors cause his death really, and in so doing, they ruined our lives and our hopes too. They were of course made able to do this by the mad inventions and lust for profits of Big Pharma. Don’t let them send you on your way too. Life is precious and there must be a way to get back to a more enjoyable one, and escape this drug damage. So much attention is being directed to it now, and people are beginning to admit what’s been going on. If ever there was a time to hold on with hope, it’s surely now. I wish Olly had been able to read what you’ve written, and write back. I think it could have made all the difference for him. Too late for him,but not for others. Thank you, and keep writing.
“Dear Doctor”
How FDA Avoided Finding Adult Antidepressant Suicidality
Furthermore, even in the rotten-apple adult studies, despite the drug company’s manipulations, Paxil (paroxetine) turned out to be causally associated with increased suicidality in depressed adults in an internal FDA review of the data. As a result, in 2006 the FDA then forced the maker of Paxil, GlaxoSmithKline (GSK), to write a “Dear Doctor” letter to all healthcare providers confirming the Paxil/suicidality causal link in adults.
https://www.madinamerica.com/2017/05/how-fda-avoided-finding-adult-antidepressant-suicidality/
In April 2006, the FDA also made the drug company put a warning in its Full Prescribing Information (label or package insert) about the risk of Paxil causing suicidality in adults with depression; but GSK convinced them to drop it in subsequent years. The warning appeared in the Physician’s Desk Reference (PDR) only once in 2007.
By
Peter Breggin, MD
May 24, 2017
About 10 years ago, my active and very productive 84 year old father had his stomach removed due to stomach cancer. Worse case scenario presented to him was that he would not be able to enjoy Thanksgiving dinner the way he had in the past. He lived for 4 more years. He was put on Reglan and left on it until I came home and recognized a Parkinson’s shuffle and terrible akathisia. He looked like a man trying to crawl out of his own skin. He also had not been able to swallow since soon after the surgery. Once we stopped the Reglan he was able to swallow and sleep although he was up and down every 2-4 hours night and day for the rest of his life. Unfortunately he was kept on many other drugs, including antidepressants and never had another productive day in his life and went on to develop a dementia that fortunately brought out his sweet disposition. I worked as an NICU nurse for 40 years and many of our infants were put on Reglan. Because it was prescribed to promote faster emptying of the stomach I always assumed that worked locally on the GI tract. Now having seen the terrible extrapyramidal side effects it has, I have to wonder how many feeding problems were actually made worse by this drug. In my opinion it should be taken off the market.