January 28 2019.
Open letter to David Haslam, NICE
Dear David,
Our paths nearly crossed at an IAPT meeting in London in 2016 but you opted not to speak in a session that had me covering “Some Questions for NICE” – a lecture covering issues that have given rise to this letter.
We brushed by each other in May 2018 when Chris Van Tulleken, in The Doctor who gave up Drugs, based on input from me, is shown contacting NICE about antidepressants and children. NICE refused to comment but claimed they were revisiting this topic.
What concerned him (me) was that pretty well everything in the antidepressants and children domain is ghost written and that every single trial including the 2 trials, which had been the basis of approval of fluoxetine for children in the US and the UK, were negative trials.
File on Four covering the same issue had the same material and message from me. They were rivetted but then claimed they couldn’t fit the material into their programme, opting instead, like Dr van Tulleken, to feature Andrea Cipriani, despite being made aware that Dr Cipriani’s work is necessarily based on ghost written material and that he had had no access to any of the data behind the studies he worked on.
Faced with difficulties in moving some substantial concerns forward, I opted for publication in a peer reviewed journal – the article is attached.
I have given a TedX talk on this topic – https://www.youtube.com/watch?v=vpTqei5hZ3g
And presented the issues in the Welsh Assembly – https://youtu.be/oku_8t8MLek
Both talks cover material presented in several national and international fora – including how the NICE process fails us – to which I can now add the following for future talks.
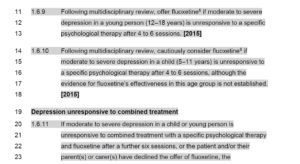
On January 23rd, an email from NICE informed me that a draft guideline on depression in children and young people was up for consultation. I was not surprised to find physicians advised in the case of more serious disorders to consider a turn to fluoxetine, or combining fluoxetine and CBT, before turning to sertraline and citalopram if these treatments fail.
Then on the afternoon of the 24th, a follow-up email indicated that sections of the guideline were blocked off from comments. These sections included those I might have commented on. Hence this open letter to you, as you personally may be unaware of the issues.
The fluoxetine trials, which were used for paediatric approval in 2001, just like the paroxetine trials a year later, were negative on their primary outcomes. FDA recognised this for both fluoxetine and paroxetine and were willing to approve paroxetine and not mention in the label that the trials were negative, leaving an unchallenged ghost-written article in the public domain to claim paroxetine worked well and was safe. Essentially the same applies to fluoxetine.
Following the fluoxetine approval, a Panorama programme made it difficult to approve paroxetine, sertraline and other SSRIs.
I am not saying these drugs should never be used. There is evidence they may produce a benefit in paediatric OCD. I can envisage using them in conditions other than OCD. But these drugs cannot be used safely unless clinicians are aware of the true state of the evidence as regards both benefits and hazards, which include making young people suicidal, wiping out their ability to function sexually, perhaps forever, or hooking them to treatments forever.
The guidance mentions that in the case of fluoxetine the risk benefit ratio has proven favourable. This seems to mean provided there might be some benefit any risks can be taken. The data do not indicate that on balance the benefits outweigh risks. There are more negative trials for fluoxetine than any other SSRI. In the case of the only notionally independent trial (TADS), the study that underpins your recommendation to combine fluoxetine and CBT, there were 34 suicidal acts on fluoxetine against 3 on placebo. I appreciate that this isn’t stated clearly in any of the 7 TADS publications but it is readily ascertained – see Hogberg et al, attached.
The guidance mentions sertraline, perhaps because Dr Cipriani recommended this for adults – on the basis of ghost-written articles and a lack of access to the data. FDA assessments suggest sertraline may be the weakest of the SSRIs for adults.
Citalopram is also mentioned as an option. Again, the data are inaccessible, the articles ghost written, and one of the key trials has I believe the highest rate of suicidal events in paediatric SSRI trials. The company then marketing it, like GSK, ended up resolving a Department of Justice action against them for a substantial amount of money.
This situation echoes 2004/2005 when NICE personnel compiling the first guideline in this area, wrote an editorial in the Lancet, Depressing Research, questioning whether it was possible to produce guidelines when trial data is inaccessible and the published literature all ghost written.
I’m not clear what the Care in National Institute for Health and Care Excellence means. It may just refer to Care of the Elderly Services. I take Care to mean there is more to Health Care than just another Service Industry – something more like taking responsibility for others as when in the care of people with diabetes we used to tell patients they needed to prick the sides of their finger when taking a blood sample as they might need the pulp of their fingers should their eye sight fail later. As a family doctor, I expect you would agree that there is always going to be a need for those of us on the coalface of clinical care to be alert to the way those who seek our Care integrate technologies, such as a drug that might make you suicidal, into a life that has to be lived.
I have not added any honorifics to your name or mine. This letter is from one person to another, not one office to another.
Yours sincerely,
David Healy
“If the scientific data is corrupted, how can a review of that literature lead to evidence based practices”?
“ The answer to that question can be found in one of the fundamental principles of evidence-based medicine, which is that those who produce Clinical Practice Guidelines should review the research literature with a critical eye “.
“They should address the quality of the studies, and discuss the limitations of the research literature and the ways that even meta-analyses may produce misleading findings”
From “Psychiatry Under The Influence”.
Whitaker R. Cosgrove L. 2015.
What a tragic missed opportunity to protect our children from the life changing, and indeed life terminating, adverse reactions caused by these drugs.
It must be hoped that any prescriber becomes fully informed and aware of SSRI induced AKATHISIA, and appreciates the association of this common iatrogenic neurotixiciy with suicidal ideation and completed suicide.
Knowledge and awareness of AKATHISIA should be a fundamental component of Vocational Training for General Practice.
The 33 page FDA – Fluoxetine Package Insert is worthy of detailed reading.
MHRA 2 NICE
Sequestered Evidence and the Distortion of Clinical Practice Guidelines
https://www.researchgate.net/publication/236726522_Sequestered_Evidence_and_the_Distortion_of_Clinical_Practice_Guidelines
At first, the MHRA’s decision to post trials on its Web site suggested that the
agency was invested in helping ensure NICE had full access to trial data.
My interview with Woods, however, suggests this may not have been the case:
LM: Would you like to see a move to a system where NICE had access to the same data as the MHRA?
KW: No.
LM: Why not?
KW: It’s important to understand firstly what NICE is there for. NICE is an NHS organization. Its job is to give advice and guidance to the NHS. I mean, the NHS is just a very large health maintenance organization.We have a statutory responsibility to the nation as a whole, and therefore our remits are somewhat different. The second thing is that is it far preferable that we are able to communicate to NICE at a confidential level, so that NICE is able for instance to organize their work programme, and to plan when a product is likely to come up for appraisal, than NICE having access to the
raw data that we see.
LM: As a former clinician yourself, as an epidemiologist, are you worried
about what people like Chalmers have talked about, which is the
general integrity of evidence bases.
KW: I know one of the things that bothers Iain [Chalmers]. And maybe this is what he has referred to. That companies submit to NICE the data they chose to submit. They submit to us, under legal obligation, all the data they have. And so, in a way, NICE is working
at a disadvantage.2
In theory, and in the view of practitioners I have spoken with, there should
be a close degree of coordination between NICE, which produces national
treatment guidelines, and the United Kingdom’s Medicines and Healthcare
Products Regulatory Agency (MHRA) which is responsible for the licensing
and post-market surveillance of all medicines and medical devices in Britain.
This is because the MHRA, as the government drug regulator, has a statutory
duty to protect U.K. consumers from unsafe treatments. Clinicians assume that
the MHRA and NICE are working in concert to ensure that treatments rec-
ommended in NICE guidelines have passed through rigorous safety standards
safeguarded by the MHRA. As the case below reveals, however, much conflict
exists between NICE policymakers and MHRA staff, conflict that in the case of
SSRIs prevented NICE policymakers from accessing clinical trial data necessary
for formulating reliable guidelines
Dear David Haslam – Stop playing Russian roulette with children lives. All your gongs and awards amount to nothing compared to one young person’s life.
So a young person with moderate to severe depression is supposed to feel better after 4-6 sessions of therapy! What does that amount to – an hour a week whatever the cause of the depression ,whether or not steps have been taken to remove or alleviate the causes . It’s like an exam – not better in 4-6 weeks – failed – take dangerous anti depressants even if we know they may make you worse or even lead to your death. David Healy is not not playing power games or politics he is talking about real human beings , Read their accounts, And you should be responding as a human being.
There is a craziness I cannot fathom.
You have a young person at risk, you have guidelines which say wait, wait and see if therapy works. You tell them you think it is working! But within 10 weeks you are on 75% doses of both antidepressants and antipsychotics, both off-label, both with suicide warnings.
And then when they don’t work everyone panics!
It really is the Keystone Cops.
Good to see a safe pair of hands!
Who shot JR?
John Read Retweeted
James Moore @jf_moore 15h
Shock as GPs hand out 67.5million prescriptions for #antidepressants, via @Daily_Express
https://www.express.co.uk/news/uk/1092207/health-news-antidepressant-doctors-mental-health-NHS-prescription
Peter J. Gordon | Hospital Doctor09 Oct 2018 11:50am
Professor Gerada has been consistent in minimising the potential for antidepressants to result in dependence and withdrawal effects. I do not understand why Professor Gerada is neither accepting evidence such as this and why she is choosing not to listen to evidence of experience.
http://www.pulsetoday.co.uk/clinical/clinical-specialties/mental-health/nice-antidepressant-withdrawal-guidance-misleading-and-without-evidence/20037572.article
Psychiatry in Fabula
https://holeousia.com/2019/02/25/psychiatry-in-fabula/
The first article I read is long, focused primarily on suicidality, Neuroleptic Drugs, Akathisia, and Suicide & Violence by Philip Hickey, blogger on Mad in America. But it is primarily an Antipsychiatry polemic collecting some clinical information and a bibliography of suicidality along the way. For example, it ends:
As I’ve stated many times, psychiatry is intellectually and morally bankrupt. They are adamantly resistant to anything resembling critical self-appraisal, and there are no depths of deception and spin to which they will not go, to suppress the reality and the consequences of their drug-pushing depredations. Neuroleptic and antidepressant drugs induce some individuals to take their own lives and/or the lives of others. Neuroleptic and antidepressant drugs are almost certainly the proximate causes of many of the mass shootings that have plagued our country for almost twenty years. How much longer can psychiatry sustain this dreadful, self-serving deception?…
http://1boringoldman.com/index.php/2016/11/30/akathisia-on-the-high-index-of-suspicion-list/
On the other hand, the other article is a new page on David Healy’s Rxisk [Akathisia by the Rxisk Medical Team] that I found both simple and clarifying:
Well done Dr Healy – and thank you
Clinches things …
Soft Power [and telling stories]
https://holeousia.com/2019/02/24/soft-power-and-telling-stories/
“We’re on the same side, really”: medical profession turns to soft power to influence policy
Simon Wessely Retweeted
Tom Moberly @tommoberly Feb 20
“You need to be at the table to be part of the discussion” Thoughts from @DacreJane @ClareGerada @SepsisUK @WesselyS @carriemacewen on influencing policymakers in my feature on “soft power” – https://www.bmj.com/content/364/bmj.l707.full?ijkey=6uyGztuJ9z36TAp&keytype=ref …
Doctors’ leaders are starting to take a different approach to winning people round to their way of thinking, Tom Moberly finds
“It was the junior doctors’ strike that really brought it home to me,” says Jane Dacre, former president of the Royal College of Physicians, of the moment she recognised that an adversarial approach to engaging with policy makers doesn’t always work.
“The mood out there was really angry and really anti-government, particularly the secretary of state. And the more that people expressed those views, the more his natural reaction was to not engage with them,” she says.
As a result of her experience, Dacre changed the way she and the college engaged with policy makers. “I observed that colleagues who are very vocal and say exactly what they think—and absolutely reflect the views of the membership and fellowship, often the more strident views—just did not get invited to discuss things,” she says.
“That sort of adversarial approach didn’t appear to get to the outcome that you wanted.”
Soft power
The approach the college sought to take instead, under Dacre’s direction, is often called “soft power.” The term was originally coined by the political scientist Joseph Nye in 1990 and used in relation to international relations. It has since been used in a broader sense of achieving influence in the absence of commanding power. Collins dictionary defines it as the “ability to achieve your goals without force, especially by diplomacy, persuasion, etc.”
Dacre credits the change in the college’s approach with helping to deliver several positive changes in the NHS. “I feel pretty confident that more money, more medical student numbers [and], lifting of visa caps were all things that we got through collaboration and soft influencing,” she says.
“In order to do your best by the members and fellows you need to be at the table to be part of the discussion to find the solution.”
Alan Milburn says that, during his time as secretary of state for health from 1999 to 2003, adversarial approaches were rarely successful. “I found personally that what worked in terms of influence was a considered conversation rather than an outright confrontation,” he says.
Those who take an adversial approach may not even get the opportunity to influence politicians, points out Nick Black, professor of health services research at the London School of Hygiene and Tropical Medicine. “Colleagues who go straight for the jugular and criticise a particular politician for coming up with a ludicrous policy get the response you can imagine from that politician,” he says.
“You’re certainly not going to be invited to come and give your views.”
Solutions and evidence
A better approach, Milburn argues, is to offer solutions. “If you’re a health minister, the last thing that you need is someone walking into your office with yet another set of problems, because you already have an in-tray full of those,” he says.
“And certainly the people that I found the most frustrating to deal with as health secretary were people who brought me yet more problems rather than those who could suggest solutions.”
An approach focused on solutions is about being helpful to achieve a common purpose, Dacre argues. “Rather than saying, ‘Don’t do it,’ say, ‘Have you thought of this?’ or ‘Why didn’t you do it like this?’ or ‘If you do it like this you’re more likely to get buy-in from our members and fellows.’
“We’re on the same side, really, in trying to get the health service improved, and the way to make progress is by just explaining that rather than being adversarial.”
Carrie MacEwen, chair of the Academy of Medical Royal Colleges, believes that evidence is key to any approach to influencing policy makers. She points out that doctors are able to provide politicians with evidence of both what is happening and what the effect of any proposed solution would be.
“That’s quite powerful: going in and saying, not only do we have experience on the front line but we’ve got evidence to support that this will work,” she says.
Telling tales
Though evidence can be helpful in influencing politicians, it rarely clinches things, argues Simon Wessely, professor of psychological medicine at King’s College London and former president of the Royal College of Psychiatrists. “Most government decisions are not made on pure scientific or doctors’ advice,” he says.
He gives the example of a discussion he had with a minister about alcohol policy. “He listened to our presentation. At the end he said, ‘Well, very good. Thank you for that. I understand the points you are making. You’ve been very helpful.’
“And then he said, ‘But, you know what, I think the lads deserve a drink.’ And, you know, that’s his job. He weighed up the options and thought, actually, we do subsidise alcohol—people have tough jobs, all that kind of stuff. That’s what a minister can do, and that’s what they should do.”
Sube Banerjee, who led the development of the Department of Health’s national dementia strategy, says that it is important to create a narrative around the change you are discussing. Telling a story about the issue can be a good way, he says, to allow policy makers and others to shift their point of view, and also to see what the next steps need to be.
“You build a story that’s coherent and simple,” he says. “You believe the story and you’re telling yourself the story. Then other people start believing it, and they start telling that story to other people. And they believe that story to be their story. They take it on. They start running with it.
“Those stories propagate and actually not only change people’s minds but also frame what the actions will look like. Because a good story tells you something about what you need to do—not just that there’s a problem but what the solutions might be—and that’s what people start selling.”
Behind closed doors
Despite the potential of a soft power approach, the fact that it relies on discussions behind closed doors and avoids public confrontations can lead to irritation and dissatisfaction. For members of representative organisations who are not privy to these discussions, this frustration may be magnified by the fact that gains made through soft power are often not announced or publicised.
Dacre says that it is important “not to gloat” when you get what you want through soft influencing approaches. “Our approach is to say, ‘It’s great that this has happened and we’ve been asking for it because it’s a really good thing to do,’” and not say ‘We won and you lost,’” she says.
This approach, particularly a lack of confrontation in the public arena, presents challenges for membership organisations, Dacre admits. “Some of the members and fellows didn’t get that,” she says. “They thought because you weren’t jumping up and down on their behalf that meant you didn’t care about them.”
Clare Gerada, who was chair of the Royal College of GPs from 2010 to 2013, says that another challenge of explaining the impact of soft power is that influence is often achieved by stopping things happening. “When I was chair of the RCGP, people often asked, ‘What does the RCGP do?’, she says. “The RCGP stops bad things happening by being at the right meeting at the right time with the right people and giving the right coherent argument.”
But the effect of this work is largely invisible to members, and so they remain unaware of these interventions by the college, she says. “The problem is you never see it. It doesn’t make headlines because the headlines aren’t, ‘College stops something happening that might not have happened in the first place.’ But that’s what you do.
“This is about the machinery of the colleges and the membership organisations, and it’s difficult for people to understand. But that is the soft power.”
A “soft power” approach also, Dacre acknowledges, means walking a fine line between having influence and being influenced. “You sometimes have to say, ‘Okay, enough,’” she says. “You sometimes have to go public with it. Because there’s a risk. The risk is that you get too close and you’re actually being manipulated.”
Dacre believes that a greater understanding of how doctors can influence policy makers would be a great benefit to the profession. “I have travelled around nearly every trust in the country, and you pick up enormous frustration about not being able to get things done, usually because of lack of resources,” she says.
“Less thought is given to how to get things done, less of a view that, ‘If we work with our organisations towards a common goal, this is what we will be able to achieve together.’”
https://truthman30.wordpress.com/2019/02/24/soft-power-and-telling-stories/
https://truthman30.wordpress.com/2019/02/27/the-serious-fraud-office-is-a-serious-joke/
“Soft power” is still power. Telling stories is not always the same as telling the truth. The shaping of policy “behind closed doors” excludes wider scrutiny. The power stays with the “narrative controllers”.
Ted …
Simon Wessely @WesselyS 17h
“Harm isn’t measured by TED talks”. Hear hear
Transparency: Revision of NICE guidance on Depression
https://holeousia.com/2018/07/12/transparency-revision-of-nice-guidance-on-depression/
http://www.niceconference.org.uk/speakers
Speakers | NICE conference 2019
http://www.niceconference.org.uk/speakers
Professor Sir Simon Wessely is Professor of Psychological Medicine and Regius Professor of Psychiatry at King’s College London and a Consultant Liaison Psychiatrist at King’s College and the Maudsley Hospitals. He is also past President of the Royal College of Psychiatrists
“I shared this communication because I am of the view that transparency matters in science and in our approach to healthcare overall. Transparency about Medical Guidelines is most important, and a powerful individual, or indeed any powerful organisation should not strive to hide matters important to public health.”
Wind Orchestra …
Kristina K. Gehrki @AkathisiaRx 7h
Music can save lives. Here’s some @PAPYRUS_tweets should want all to hear: https://rxisk.org/akathisia/ @billiamjames
https://rxisk.org/akathisia/
Akathisia (I Can’t Sit Still), is also available on iTunes, Spotify, Amazon and Google Music.
Another Family Blame Lundbeck Drug for Brother’s Death.
https://leoniesblog.com/2019/03/02/another-family-blame-lundbeck-drug-for-brothers-death/
Published by Leonie
2 March 2019
“Meanwhile, the drug regulators, in place largely to protect us, ignore the rising body of evidence and bury their heads in the sand. The families shouting ‘stop’ however, are constant.”
MH 2 MH
What is worrying about this ‘Fight Fake Heath News’ blanket today in the Scottish Mail on Sunday is Matt Hancock and Simon Stevens :
“Needlessly risking people’s health by spreading reckless and ignorant misinformation claiming otherwise is completely unjustified’
‘These kind of pernicious lies have no place in our NHS
On Friday, NHS Chief Executive Simon Stevens warned that ‘vaccine deniers’ who went online to spout ‘fake messages’ were making it harder for doctors to ‘win the public argument’ on vaccination.
He told a meeting at the Nuffield Trust think-tank: ‘The vaccination deniers are getting some traction.
Although nine in ten parents support vaccination, half of them say they have seen fake messages about vaccinations on social media.’
https://www.dailymail.co.uk/news/article-6764823/Doctors-peddle-myths-effectiveness-statins-putting-lives-risk-says-Minister.html
https://www.dailymail.co.uk/health/article-6764117/Devastating-investigation-reveals-impact-deadly-statin-denier-propaganda.html
Professor Sir Rory Collins, the British scientist behind pivotal research into statins, says the potential consequences far outweigh that of the infamous MMR vaccine scandal, in which disgraced paediatrician Andrew Wakefield fabricated evidence to support his idea that the jab triggered autism in infants, leading to a decline in vaccination uptake and the resurgence of measles. The suggestion is that the statin deniers are simply wrong rather than dishonest, but Prof Collins says: ‘In terms of death and disability that could have been prevented, this could be far worse than we saw with MMR.’
In a recent blog Dr Kendrick wrote: ‘Professor Sir Rory Collins and Professor Colin Baigent made a pact with the dev… sorry… they made a pact with the pharmaceutical industry to take hold of all the data on statins. They will not let anyone else see the data they hold. Including all the data on side effects.’
Responding to our investigation, Dr Kendrick added: ‘I believe people are being conned, deliberately misled. All industry-funded studies were positive. This is either a remarkable coincidence or something else.’
Cholesterol Games
3 March 2019
Scottish Doctor
https://drmalcolmkendrick.org/
‘Anyway, this is probably enough for now. I just wanted to give you some idea of the attacks and battles that are gong on and to shine a little light on what happens. The Mail on Sunday have published a very long article attacking ‘statin deniers’ with pictures of me Zoe and Aseem at the front. I think I look quite dashing. Not as dashing as Aseem who is a very handsome swine, and also young, and intelligent – and brave. Yes, I hate him.
Nor am I as attractive as Zoe Harcombe. But hey, at least I got my picture in the national press. I wasn’t very keen on the bit where they called me self-pitying. But I was quite pleased that they included some of the stuff that I sent.
Until next time, best wishes from the mass-murdering, statin denying, self-pitying Dr Kendrick.
In the Current NICE guidelines, if a young person or parent says NO to drug therapy than 15 weeks of alternative therapy is recommended. After 6 weeks of therapy if the depression is still there Pills are pushed.
In my former teaching Career, I did drugs education with 6-16 year olds. On the Curriculum there were drugs galore…..some legal…some illegal. Alcohol, Cigarettes, Cannabis, Amphetamines were all there, as was Valium.
Given that Anti-depressants are known to be potentially harmful, Why are they not on the curriculum?
Anyone with a duty of care to those under 16 surely should be allowed to let them know, they can say NO. A word, Gps, Psyches and P(harma) in many cases are incapable of uttering.
DH…thank you DH….Will You say No……..
Dr Healy,
Thank you for continuing to highlight the scandal of the inaccessible data on these SSRI drugs, and the continuing controversy of their (over) use and general harms that they cause.
The long term damage of these drugs is scandalous also.
Most people prescribed psychiatric drugs long term seem to have their lives cut short, even if they come off the drugs after many years on them. The toll on the body and nervous system from these drugs is hard to quantify, and it’s not being documented- apart from serious studies such as Robert Whitaker’s ‘Anatomy Of An Epidemic’ and Tha work of Mad In America…
https://truthman30.wordpress.com/2019/03/04/in-memory-of-paul/
In Memory Of Paul…
I met Paul 15 years ago in an online support group for Paxil (Seroxat) sufferers. He passed away over a week ago, and his funeral was last week. I couldn’t make the funeral as I couldn’t afford the trip which would have entailed a boat, and a train and other expenses that I just don’t have to spare at the moment. That’s what happens when a dodgy prescription drug destroys most of your life. You end up with scant finances – sometimes- also- for life.
So much is -forever affected.
Paul was 61 when he died. He had been off Seroxat for about 10 of those years, but had been on it 14 years. I was on Seroxat for about 4 years, and I was ravaged, Paul’s horrible Seroxat experience was beyond- what even I- could hardly imagine. He suffered in so many indescribably inhuman ways; cruel, painful ways which he would often try to articulate to me, but sometimes he was so traumatized he couldn’t speak, and he hid away.
It’s odd when you are damaged by a prescription drug like Seroxat, as your life is forever tainted by the experience. Paul’s marriage was also affected, and his relationships with his kids, and his friends. He lost his work, his health, and his income, but a drug like Seroxat takes more than that- it takes away your identity, your soul, and your sense of self (those things are beyond any price).
Paul was acutely aware of what he lost through his horrific time on the Seroxat poison and we would often talk about it. In fact, we would talk about it a lot. We had ‘Seroxat’ in common, but we also had music in common, and our love of our guitars. Paul was extremely talented; both a highly skilled a musician, and producer. Had Seroxat not destroyed his nervous system, he would have been inundated with work, as he was the most sought after guitar teacher in the region where he lived (he was that good) but what little he could do after Seroxat- was a struggle for him- but he really tried.
He tried so damn hard.
I stayed with Paul, and his wife, several times, in their remote house, in rural Wales, and despite his agonizing condition, we had truly great belly laughs, and we had great times. They were without a doubt, among the most kindest, humble, and genuine people I have ever met. What little they had- they shared. His wife Sarah- is an amazing cook, and so obliging .
They were what I discovered to be- the true meaning of ‘ the salt of the earth’ people.
Paul’s life was cut short because 14 years on Seroxat, and years of protracted withdrawal (that he never fully recovered from) meant that his quality of life was severely diminished for his remaining years.
He had a heart attack, at 61. That’s too young to die.
Paul and I would often discuss GSK and Seroxat, and he was well aware of the evil which had come into both of our lives through that vile blue pill. We had hours upon hours of discussions about it all.
I hope he is at peace now.
RIP friend.
See you in the next life.
Thanks Truthman, and thanks Paul.
Yet another soul lost, mine will join his ranks, someday, sharing the same fate.
Your words about Paul inspires me to fight back. My stomach turns with the thought of dieing without letting GSK know what they have done.
And if you think that way, in a fight you can’t ‘win’, you can neither ‘lose’.
Ove2019
That article with the talking heads yoking statins and MMR makes me wonder at where such catastrophic lack of self-awareness comes from. Once completely unrelated scandals start being yoked together like this — the stakes of the conflict are no longer to damage the credibility of vaccines or statins or psychopharmacology but of medicine as a whole. It’s at the very least bad and self-destructive PR. This way, when something does blow up it causes incredible collateral damage.
The reputation of modern medicine rests on a couple of serendipitous discoveries that seem to work like magic and the careful accumulation of practical knowledge. The careful accumulation of practical knowledge bit seems to be thrown away now in favour of policies enacted from 50,000 feet and trying to earn respect for the policies by yoking their credibility to the credibility of medicine as a whole. It won’t work because anyone who pays attention will not respect a doctor who is no longer exercising independent professional judgement (could be wrong, but takes input when necessary) but rather is passively transmitting guidelines prepared by the ‘real’ decision makers who are inaccessible (and always defined to be right, so don’t try to communicate a data point suggesting otherwise). As for such ‘if you disrespect statins you disrespect all science’ ploys, this is like trying to hide toxic waste by diluting it into a swimming pool. It works if you have one cup of waste so no one is the wiser, but when everyone gets the same idea suddenly no one wants to swim in that pool. Meanwhile talking heads run around the perimeter shouting “how dare anyone not want to swim in this pool! We’ll have you know it contains more than 50% H2O! Do you deny the efficacy of H2O as a swimming medium?!” Yes, it will probably suck, and it will be a terrifying waste of what could have been clean water, but if people are pushed into an impossible situation long enough they can opt to live without (most of) modern medicine, just as they could opt to live without swimming pools, and have in the past. Enough people doing this and then every branch of medicine, not just vaccinators, will be writing articles about how their patients need to be rounded up by the government.
Also the notion that people who mostly cite 50,000 foot statistical studies have a grasp of the definition of the word ‘healthy’ starts to sound incredible. Ultimately, apart from a small (and hugely overstated — another vector for rhetorical abuse) number of mad people, only the patient can judge if the intervention is making them healthier. The doctor sees the patient for a few minutes but the patient lives with themselves 24hrs a day.
Dr Maryanne Demasi @MaryanneDemasi Mar 8
Statin Island http://www.pulsetoday.co.uk/views/blogs/dr-kailash-chand/statin-island/20038348.article#.XILUwHBYou0.twitter … Honorary vice president of the British Medical Association (BMA) @KailashChandOBE responds to negative press about those who question statins @DrAseemMalhotra @zoeharcombe @malcolmken @jsbamrah
Statin Island
Dr Kailash Chand
Last Sunday, The Mail on Sunday published an article on ‘the statin deniers’, without, in my view, ascertaining crucial facts. When drug industry-sponsored trials cannot be examined and questioned by independent researchers, science ceases to exist and becomes nothing more than marketing.
http://www.pulsetoday.co.uk/views/blogs/dr-kailash-chand/statin-island/20038348.article#.XILUwHBYou0.twitter
Dr Maryanne Demasi @MaryanneDemasi 40m
Good morning Copenhagen. Looking forward to the Symposium tomorrow. My talk is on clinical trial bias, lack of data transparency & censorship!
Many eminent psychiatrists, such as Peter Gøtzsche (left), believe that antidepressants should never be prescribed to children.
However, even if we accept that there may be situations in which it might benefit a child to be prescribed Fluoxetine, this was clearly not one of them. To inflict an SSRI drug with links to suicide on to a slight, underweight schoolgirl is reckless in itself, but then to double the dosage is completely indefensible.
http://antidepaware.co.uk/ellie-aged-15/
Prof. Peter Gøtzsche @PGtzsche1
Institute for Scientific Freedom, inaugural meeting 9 March in Copenhagen. Seats still available, see programme and how to register here: http://www.scientificfreedom.dk
https://www.scientificfreedom.dk/
Clare’s Chairs and the Care Quality Commission
Clare Gerada Wessely is to become the Clinical chair of the NHS Assembly – described as ‘;usual gang of gong chasers who avoid contact with patients’ and ‘a ghastly gang of parasites’ by anonymous commentators. how she has managed to bag the CLINICAL chair on a politically led project is hardly surprising as Clare is a well known denier of the extent of harms caused by prescription drugs – even though as Pulse med mag states -‘she has helped 1000’s of drs recover from mental illness and get back to work’ and therefor could hardly have missed some of the harms . But it’s a good point in support of her plan to grab more money to set up another tax funded confidential samaritan type helpline for GPs.when so many GPs are getting out or not even getting in to practice.
At the same time the Care Quality Commission is telling people to Complain about GP Care to Improve Services. Cat among the pigeons or paper tiger.? Seems they needed to conduct a survey to find out why over half of those people who wanted to complain don’t. Many of those who have even heard of the CQC or who have been through the system will be very cynical about trusting the CQC on their past horrendous record of letting vulnerable people down time after time..
GR – Head of Policy and Campaigns, RCPsych
Minutes and slides available of APPG meeting on 7 Feb 2019
http://prescribeddrug.org/wp-content/uploads/2019/03/APPG-Meeting-Minutes-070219.pdf
LM raised NICE withdrawal commission – Paul Chrisp has confirmed that it is the aim for this to build on the PHE review, and PHE & NICE have talked about aligning the pieces of work. 3. Update on conversation with RCPsych Members of the secretariat met with Wendy Burn, President of the RCPSych in November and discussed a number of issues.
As a result of the meeting WB and GR will be visiting the Bristol and District Tranquiliser Project (BTP) this month.
JD is following up with Carmine Pariante, Professor of Biological Psychiatry of Kings College London, re research gaps.
GR advised the college is developing its policy on antidepressants and a leaflet on coming off them and intends to involve patient groups in the latter. RCPsych is also considering creating a podcast to promote its new policy position and leaflet to tease out some of the complexity and challenges on this issue.
The group invited GR to attend the next meeting to update on progress.
It was agreed that the group would like to make contact with the RCGP along similar lines.
“It is part of the professorial tradition for some that they are allowed to write whatever they want according to their prejudices”
https://holeousia.com/2019/03/05/i-had-dinner-with-william-sargant/
John Read @ReadReadj 7m
John Read Retweeted James Moore
Tomorrow (Weds) Radio 4 – ‘PM’ programme (5pm-6), in an extended news item Sarah Vine interviews people about withdrawal from antidepressants, inc. James Moore and myself.
This issue is now well and truly in the public domain. Well done all concerned!
https://twitter.com/lewis_louisa
Reasons to Be Cheerful?!
Just caught a follow up programme on R4 PM on Anti depressants
will be on BBC SOUNDS at 17:17
points raised included withrawal discussion by James M and Sarah V, that people in deprived areas are being over prescribed, GP contribution gave usual reasons/excuses – no other option except drugs, (no contribution from the usual slippery spokespeople from college of GPs or Coll of psychs, ) out of date guidance , too little attention to social circumstances, too little research. Oliver Letwin chair of parliamentary cttee admitted that as he pointed out there has been resistance as the situation was not properly understood (hmm) and once the problems are better understood things can be quickly resolved. He emphasised several times that different ways of doing things, including expert advisers are being considered. There were a lot of good points made in the interview although
nobody mentioned lack of data from drug companies so that as David Healy keeps pointing out both prescribers and people prescribed for can weigh up the rxisk. Hope this isn’t a deliberate ommission.
and another followup tomorrow focusing on women and anti depressants at the same time R4 PM.
.
How to Quit Antidepressants: Very Slowly, Doctors Say
By
Benedict Carey
March 5, 2019
https://www.nytimes.com/2019/03/05/health/depression-withdrawal-drugs.html?register=email&auth=register-email
Mustering solid evidence, two psychiatrists have denounced their field’s standard guidelines for how best to wean patients from depression medications.
Thousands, perhaps millions, of people who try to quit antidepressant drugs experience stinging withdrawal symptoms that last for months to years: insomnia, surges of anxiety, even so-called brain zaps, sensations of electric shock in the brain.
But doctors have dismissed or downplayed such symptoms, often attributing them to the recurrence of underlying mood problems.
The striking contrast between the patients’ experience and their doctors’ judgment has stirred heated debate in Britain, where last year the president of the Royal College of Psychiatrists publicly denied claims of lasting withdrawal in “the vast majority of patients.”
Patient-advocacy groups demanded a public retraction; psychiatrists, in the United States and abroad, came to the defense of the Royal College. Now, a pair of prominent British psychiatrists has broken ranks, calling the establishment’s position badly mistaken and the standard advice on withdrawal woefully inadequate.
In a paper published Tuesday in the Lancet, the authors argued that any responsible withdrawal regimen should have the patient tapering off medication over months or even years, depending on the individual, and not over four weeks, the boilerplate advice.
The paper is by far the strongest research-backed denunciation of standard tapering practice by members of the profession.
“I know people who stop suddenly and get no side effects,” said Dr. Mark Horowitz, a clinical research fellow at Britain’s National Health Service and King’s College London, and one of the paper’s authors.
But many people, he said, “have to pull apart their capsules and reduce the dosage bead by bead. We provided the science to back up what they’re already doing.”
The field of psychiatry has conducted few rigorous studies of antidepressant withdrawal, despite the fact that long-term prescription rates in the United States and Britain have doubled over the past decade, with similar trends in other Western countries.
More than 15 million Americans have taken the medications for at least five years, a rate that has almost more than tripled since 2000, according to a New York Times analysis of federal data.
Outside researchers who have studied withdrawal said the new paper was a welcome contribution. “I think what they’ve presented really reinforces what I’ve observed in clinical practice in many patients, and it’s almost identical to the tapering regimen I use,” said Dr. Dee Mangin, the chair of family medicine at McMaster University in Canada, who was not involved in the paper.
Dr. Mangin, who is completing her own two-year study of Prozac withdrawal, added, “The other important thing is that it validates patients’ own reports of their experiences. It’s tremendously frustrating when patients describe a different experience than physicians expect, and don’t feel they’re being heard.”
Dr. Horowitz and his co-author, Dr. David Taylor, a professor of psychopharmacology at King’s College and a member of the South London and Maudsley N.H.S. Foundation Trust, decided to address the topic in part because of their own experiences with medication.
Dr. Horowitz said he had severe withdrawal symptoms after tapering down after 15 years on antidepressants. Dr. Taylor had previously written about his own struggles trying to taper off.
The two psychiatrists began by visiting online forums in which people on antidepressants advised one another how best to withdraw. Those sites consistently recommended “micro-dosing,” reducing doses by ever smaller amounts over months or years, sometimes by removing one bead at a time from capsules.
The two researchers dug into the literature and found a handful of studies that provided evidence for that method.
In one 2010 study cited in the new paper, Japanese researchers found that 78 percent of people trying to taper off Paxil suffered severe withdrawal symptoms. The research team had them taper much more slowly, over an average of nine months and for as long as four years. With this regimen, only 6 percent of subjects experienced withdrawal.
In another study, Dutch researchers in 2018 found that 70 percent of people who’d had trouble giving up Paxil or Effexor quit their prescriptions safely by following an extended tapering regimen, reducing their dosage by smaller and smaller increments, down to one-fortieth of the original amount. This is the regimen recommended in the new paper.
Dr. Horowitz and Dr. Taylor also cited brain-imaging evidence. Antidepressants such as Paxil, Zoloft and Effexor work in part by blocking the serotonin transporter, a molecule that works in the synapses between brain cells to clear out the chemical serotonin, which is thought to help impart a sense of well-being in some people. By blocking the transporter, antidepressants prolong and enhance serotonin’s effects.
But the brain-imaging studies found that inhibition of the transporter increases sharply with addition of the drug and, by extension, also drops sharply with any reduction in dosage. The standard medical advice, to reduce dosage by half — for instance, by taking a pill every other day — and end medication entirely after four weeks, does not take this into account, the two researchers argued.
“Doctors have in mind that these drugs act in a linear way, that when you reduce dosage by half, it reduces the effect in the brain by a half,” Dr. Horowitz said. “It doesn’t work that way. And as a result, there’s a huge load in terms of the effect on brain receptors, and patients are being advised to come off way too quickly.”
Laura Delano, executive director of Inner Compass Initiative, a nonprofit organization that runs The Withdrawal Project and focuses on helping people learn about safer psychiatric drug tapering, said: “I didn’t know about the benefits of slow tapering when I came off five meds in five months, and had a very difficult time in withdrawal.”
The new paper, she added, “speaks to how hard it is to get this information into the clinical world. We laypeople have been saying this for a long time, and it’s telling that it took psychiatrists coming off meds themselves for this information to finally be heard.”
Dr. Horowitz and Dr. Taylor called for more, and more careful, research to be done on withdrawal, to bring their field up to speed, and to develop withdrawal strategies tailored to individual patients and individual drugs.
“I think psychiatrists are taught to learn things from textbooks and from well-conducted studies,” Dr. Horowitz said. “We don’t have many of those for withdrawal, so it makes it hard to believe it’s real. And psychiatrists spend a lot more time prescribing things than stopping them.”
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(19)30032-X/fulltext#.XH-GaU2U27w.twitter
BOB FIDDAMAN @Fiddaman 9h
Pariante was interviewed on BBC Radio 4 today after the subject of brain pellet withdrawal once again made the news in the New York Times. https://fiddaman.blogspot.com/2019/03/life-saving-evidence.html … #BrainPellets
https://fiddaman.blogspot.com/2019/03/life-saving-evidence.html
OL – Did He?
recovery&renewal Retweeted
James Moore @jf_moore 3h
Replying to @BBCPM @EvanHD @ParianteSPILab
We are very glad to hear that the voices of patients are finally getting clearly heard in the #antidepressant withdrawal debate, so my question is, when does this translate into action?
James Moore Retweeted
CEP @CEP_UK 10m
Right now, Sir Oliver Letwin doing a fantastic job on BBC Radio 4 making the case for far more recognition and support for people whose lives have been blighted by prescribed drug dependence and withdrawal.
Sorry to rain on the parade, but, I think we know completely where we are with AD withdrawal; aggression, violence, homicide and suicide.
Kristina K. Gehrki @AkathisiaRx 21h
Thanks for sharing this. I didn’t hear any mention of SSRI side effects nor withdrawal-induced deaths on today’s radio program. No surprise here as I’d bet my house that these prescribers also don’t mention such when prescribing.
The follow up on Friday was publicised as focusing on women and depression. And why so many women are prescribed them.
The presenter was a man.The introductory contribution was from a man – a male clinical psychologist who was positive about using drugs for clients
then two other men had e mails read out – both reliant on anti depressants they didn’t think they could manage without- then Tony Kendrick an ‘expert’, another man -all with positive messages about AD’s –
The programme then led into a discussion of the pressures on womens’ lives by three women wittering away ending up with S Vine declaring with a chuckle that the end of her stressful day is helped by drinking gin. Was the producer got at? There was no discussion about the high prescribing of anti depressant to women at all. At least if not providing info about when the action was to begin on changing the services there was some honest cticisism and truth telling on the previous days programme.by Oliver Letwin.
.
It would be interesting to find out whether there are more women complaining about withdrawal effects compared to men – it would make sense if women are prescribed more anti depressants. this programme showed where a programme was supposed to be about women prescribed anti depressants a crafty sidelining went on with the inclusion of two male ‘experts’ a male presenter leading the discussion only one woman e mailer who was also positive ‘benfitted enormously’and three women who avoided any mention of drugs and their effects on womens’ lives –
The programmes can be played back on R4 BBC SOUNDS
Depressed patients stop pills too hastily, GPs told
https://www.thetimes.co.uk/article/depressed-patients-stop-pills-too-hastily-gps-told-20f7vtmsk?utm_medium=Social&utm_source=Twitter#Echobox=1552289322
Chris Smyth, Health Editor
March 11 2019, 12:01am, The Times
Coming off antidepressants can take months and doctors must not rush patients into stopping, experts say.
Patients benefit from tapering off the drugs over nine months to avoid getting trapped on the medicines by debilitating withdrawal symptoms, they argue.
Brain scans show that current methods of stopping can lead to abrupt changes that could be avoided with more gradual dose reductions, according to a review of research published in The Lancet Psychiatry.
More than seven million people in England are on antidepressants and the number has been rising. They have been shown to work for severe depression but many patients experience withdrawal symptoms. Critics of current methods say these are often mistaken for the return of depression, leading to people being put back on medication long term.
A review into the problem has been beset by rows and current guidelines recommend halving the dose for four weeks before stopping to avoid symptoms.
However, David Taylor of King’s College London and Mark Horowitz, a training psychiatrist at the Prince of Wales Hospital in Sydney, argue that this is wrong. “When you halve the dose of your antidepressant once you don’t decrease the action of the drug very much at its target receptors. But when you reduce the drug to 0mg from half the dose you go down a huge amount in effect at receptors,” Dr Horowitz said.
“We suggest that this is why people get into trouble when they taper — they are going down too fast. We therefore suggest that patients should halve their dose a number of times before stopping, which will mean the drop in effect at receptors is much more gradual.”
He proposes halving doses six times over many months, arguing: “There is no downside to doing our technique. All we are saying is go slower.” Dr Horowitz, who struggled to come off antidepressants himself, added: “If I hadn’t had my own experience of this I wouldn’t have believed it either.”
Professor Taylor said: “Doctors and patients need better evidence on how to taper people off safely and carefully.”
James Davies of the Council for Evidence-based Psychiatry, a critic of current methods, said: “We have sufficient evidence to update our guidelines. . . for many people a 2-4 week taper is far, far too fast and very dangerous.”
Carmine Pariante of the Royal College of Psychiatrists said: “When withdrawal is properly managed, most patients can come off them with minimal side-effects or with side-effects that can be managed with the help of their doctor, by slowing or stopping over four weeks. However, we know this is not the case for all patients . . . While this paper is an important theoretical contribution, the recommended protocols will need to be tested to ensure they work.”
‘The college was always clear there was a problem with antidepressant withdrawal, …
Proof that getting off depression pills without crippling side-effects can take MONTHS
Anxiety, electric shock sensations and insomnia are some withdrawal symptoms
Drugs in question are common selective serotonin re-uptake inhibitors (SSRIs)
These include fluoxetine (brand name Prozac) and citalopram (Cipramil)
https://www.dailymail.co.uk/health/article-6797517/Proof-getting-depression-pills-without-crippling-effects-MONTHS.html
By Jo Waters
12 March 2019
James Moore
Caldicot, WLS, United Kingdom
12 Mar 2019 —
The antidepressant withdrawal debate has been reignited recently, partly by the appearance of a scientific paper in The Lancet Psychiatry and an accompanying piece in the New York Times. For me personally, the most interesting aspect of the paper is that both authors have reported their own experience of withdrawal effects.
Please have a read if you can spare the time and please share on social media too, we need more signatures and this will help.
http://www.letstalkwithdrawal.com/withdrawal-does-not-discriminate/
Thank you for your support and your signatures.
James
https://www.change.org/p/provide-tapering-strips-to-help-users-who-want-to-stop-taking-anxiety-depression-drugs/u/24280388?cs_tk=Ak5J7vYJj5CbA-2Bi1wAAXicyyvNyQEABF8BvFvzxNCcbwvOIaE3Ub-XgsI%3D&utm_campaign=40063a1214a04cac91ac673fdfb6bda1&utm_medium=email&utm_source=petition_update&utm_term=cs
Withdrawal Does Not Discriminate
March 11, 2019
JM Moore
Let’s Talk Withdrawal
http://www.letstalkwithdrawal.com/withdrawal-does-not-discriminate/
The ‘Pilgrim’s’ Progess …
No Man Is An Island… (not even a retweet)
Jo Waters, entertains …
https://twitter.com/Appledorianiexp
James Moore @jf_moore 32 mins
Replying to @ParianteSPILab @Appledorianiexp @rcpsych
It shouldn’t take journalists/campaigners to force your hand. RCPsych’s ‘position’ until recently was ‘most people have no trouble’ Change is the result of campaigning by people who are sick from withdrawal and should be taking care of themselves, not having to educate psychiatry
Carmine M. Pariante Retweeted
Carmine M. Pariante @ParianteSPILab 12h
Thanks Jo Waters @Appledorianiexp for the opportunity to put across @rcpsych view: for some people, the four-week recommendation is not enough, and they need to have progressive reduction of the dose of their antidepressants to a small dose, and over a much longer period.
I think ‘we’ get the picture
https://twitter.com/ParianteSPILab/status/1105582610519130112
Jo Waters @Appledorianiexp 12h
Replying to @ParianteSPILab @rcpsych
Thank you for your analysis
Three-piece-suite
I think WesselyS and GeradaC and BurnW are pretty happy to take a back seat and let ParianteC do all the talking… what is clear is that BurnW is not the go-to person, as Wessely-Was, having put her foot in it very publicly, and it is obvious it is a collective decision and Carmine is in receipt of ‘Island’ status …
Clare Gerada #FBPE @ClareGerada 5h
Very reassuring information from @gmcuk . For vast majority of doctors GMC doesn’t need to know if you have a health problem (including mental health) as long as seeking appropriate help & not putting patients at risk.
https://holeousia.com/2019/03/12/from-the-individual-to-the-institution/
Citizens need to to take care what they reveal to medics. During a consultation all sorts of information may be disclosed not realising it can be passed on or be permanently recorded .There have been umpteen breaches of confidence already and a new project between the NHS and DWP (dept of work and pensions)doesn’t bode well when some GPs are expressing outrage others support it – who knows which doctor they will end up with, what advice and information about ‘sharing info’one medic will give compared with another.
Re Pulse Med Mag:- The Government Could Get Automatic Access to GP Patients’ Records As Part of a Digital System for Welfare Application Assessments’.
DWP ‘We’re building a digital service to gather information from citizens and present them to DWP processing agents’. (Even the terms they use are cold and inhuman).
Maybe Clare GeradA- Wessley was aware of the project which is runNing a pilot somewhere already – she is giving the message to medics that their own health records should be more protected than those of the rest of us. Medics and other health workers do need to be cautious though – very little can be kept totally confidential even if using the services run by Clare G and colleagues – someone is accessing them and assessing them..Individuals can choose to refer any concerns to the GMC or the Care Quality Commission themselves of course. Is C G really giving medics the best message by telling them to keep their own mental health problems secret? They don’t live on another planet and when word get around they are often shown much respect and compassion by those who consult them.
Some GPs and other well paid citizens could keep their information private from agencies of course as they will not always need to claim welfare . Everyone else has to rely on the tosh given out by the government – ‘no information would be accessed without explicit and informed consent’.
David Healy Retweeted
Mischa Anna Selis @miepsja 22h
Mar 13 Translational neuroscience lecture: Responsible care and neuroscience – @DrDavidHealy @MaastrichtU
Interview
Van bijna alle medicijnen die de afgelopen dertig jaar zijn ontwikkeld, zijn de schadelijke effecten niet goed bekend. Dat stelt de Britse hoogleraar psychiatrie David Healy in reactie op de ophef in Nederland over pijnstiller oxycodon en het antidepressivum seroxat.
https://www.trouw.nl/samenleving/-er-wordt-gesjoemeld-met-data-bij-vrijwel-alle-medicijnen-~a2daeb88/
Healy was involved in research into seroxat and similar medicines, and is known as a fierce critic of the pharmaceutical industry. “The information on medicines in scientific articles is currently the largest package of fake news in the world,” says Healy. He will speak at the University of Maastricht on Wednesday.
How many medicines do you think do more harm than good?
“Every medicine is essentially harmful. That is why we limit the use of medicines to people who have something harmful among their members. We must always weigh the problems they have due to their illness against the problems that the drug is likely to cause. A medicine therefore consists of two things. One is the combination of chemical substances, and two is the information that comes with that medicine. If you are going to take a risk by taking a medicine, you need to know how great that risk is.
“The wave of medicines that came on the market in the 1940s and 1950s saved lives, which is beyond doubt. The clinical research then came from doctors who prescribed the drug and saw for themselves what the effect of a drug was. After that, more and more clinical tests were commissioned by the pharmaceutical industry. Doctors started to trust that information. A large part of the recent medicines probably does more harm than good, but we don’t know. ”
You investigated the seroxat study. What was wrong there?
“We were given access to the data from one of the tests in the 1990s, study 329. On the basis of that research, it was concluded that the drug worked well in young people. Our analysis of the raw data showed that the drug did not work well, and that a large group even became suicidal. What happened here happens with practically every patented drug. Only the data that demonstrates that the medicine works, or that can be edited to prove it, will be published. Indications that a medicine does not work or is even dangerous are not mentioned. ”
How is that possible?
“Practically all clinical experiments that have been published in the scientific journals since the 1980s lack the data on which the article is based. The official authors have not seen that data. Behind them, a ghostwriter is hiding at a company that supplies medical supplies that is paid for by the pharmaceutical company. That ghostwriter did not see the raw data either. Another company, which performs clinical tests, provides an overview of part of the data. That company knows what results the pharmaceutical needs. ”
Minister Bruno Bruins wants to reduce the use of oxycodone. How can he do that?
“Not by saying that he wants to reduce the use of oxycodone. The mention of a concrete means only works as marketing. We should all no longer take medicines that have been on the market since the end of the 1980s, unless pharmacists make public the raw data of their clinical research. So that everyone can check the operation. ”
How realistic is that?
“We have more power than we think. If patients, doctors and politicians join forces, the pharmaceutical industry must contribute. In the 1980s, people in the United States took less than one pill a day. Today, the average person over 45 takes three or more pills a day, and the average person over 65 takes five or more. The situation is similar for us in the United Kingdom. Life expectancy has recently fallen in both countries. I think that is due to the use of medication. It requires guts, but something has to change. ”
Expert in side effects
David Healy is a professor of psychiatry at Bangor University in Wales. He is an expert in the field of drug side effects, and acts worldwide as a witness in court cases where suspects may have committed violence under the influence of drugs such as seroxat. On the rxisk.org website, he collects information about side effects from patients.
Wonderful, Wonderful Copenhagen – (an old song by Danny Kaye)
It’s more than time the college of psychiatrists was abolished – they are trying to do a damage limitation by commandeering the work done by those who have been exposing their practices as harmful deceitful and downright dangerous. – at times willfully denying the evidence provided by David H and others and using bullying tactics to attempt to undermine and silence them. Citizens need something, people they can trust but it won’t be on the level of the group led by Carmine Pariente either .He joined ‘Medium’ on Feb 2019 (see website) to combat the negative image of psychiatry by publicising his and the team of carminites work at institute of psychiatry
The cringeworthy article is published by C P in ‘Inspire The Mind’ the official publication of the research group. – ‘everything you have wanted to know about mental health the effects on the brain and the body and the science behind it’. How we use people as research fodder then hide the evidence – that might be the next piece for his publication.
By the way… SPILab… InSPIre the Mind… is the wordplay clear?!
https://medium.com/inspire-the-mind/inspire-the-mind-of-the-medium-community-and-beyond-e9109f7c9586
There is good news too.
Celebrities have been very brave in describing their own experience of mental health problems, often using their live acceptance speeches when they receive an award. Lady Gaga, Letitia Wright, Kesha, Selena Gomez and Gabrielle Union are just some recent examples, but the royal family has been doing this for years, with the personal accounts of Prince Harry and the Duke of Cambridge on the impact of their mother’s death, and the vocal campaign by Kate Middleton against stigma.
The brain of people with mental disorder was until recently a big black box, that we are just now starting to understand.
Sometimes it is difficult to navigate the headlines, even from patients’ account: for example, antidepressants are described both as life-saving and as life-wrecking.
Sounds like Mystic Meg on a Bad Day, Susanne..
The name dropping, the crude ‘patients’ accounts, the medium and beyond; he has surpassed himself with his hoops and earings and glass balls, the ‘wheel’ of destiny … ?
2 B or not 2 B
NICE guidelines on antidepressants are soon to be rewritten, and it’s likely they will now take into account the difficulty of stopping such medication.
Millions of patients have been vindicated. The medical profession owes them an apology.
The interaction in most appointments is NOT a dry, polite exchange (as the previous Comments attest), it’s a regular mugging, an assault on client’s rights, health, & short & long-term safety; shrieking, contorting, on-your-knees suffering.
https://www.dailymail.co.uk/health/article-6815715/DR-MAX-MIND-DOCTOR-antidepressent-torment-ISNT-mind.html
https://www.madinamerica.com/2019/03/clients-solicit-medication-changes-psychiatrists/#comment-151110
Krista Hartmann March 16, 2019 at 2:52 am
My goodness, Ms. Morrill, this self-important, naval-gazing, “studying”, “examining”, & “analyzing” research is darkly hilarious.
All this verbal mincing around the client’s “lack of opportunity to make explicit requests” is insulting to many in the ‘trenches’.
With respect…and real-life insight gained from 11 years of private & state-funded psychiatry, coast to coast…may I suggest you apply your study of “the impact of social violence” directly to the topic of this specious little report.
Were you ‘just sharing’ or do you think this tepid, pearl-clutching is significant somehow to anyone outside of the zone of academia?
The interaction in most appointments is NOT a dry, polite exchange (as the previous Comments attest), it’s a regular mugging, an assault on client’s rights, health, & short & long-term safety; shrieking, contorting, on-your-knees suffering.
This article’s attempt at sanitizing this “social violence” (your field) at med checks in the name of mental health care, is mightily offensive. There is no respectful listening to a client, no responsive actions taken, just ‘cost & liability’ considerations.
Side effects are authoritativly declared trivial or (clients ALL know this by heart)-SYMPTOMS. And that’s a Full Stop.
There, mystery solved….now ‘study’ how to, psychologically of course, supress the conflict-of-interest gene in psychiatrists; nature or nurture? Talk among yourselves.
We’ll be waiting right here.
Peer-Support Groups Were Right, Guidelines Were Wrong: Dr. Mark Horowitz on Tapering Off Antidepressants
In an interview with MIA, Dr. Horowitz discusses his recent article on why tapering off antidepressants can take months or even years.
https://www.madinamerica.com/2019/03/peer-support-groups-right-official-guidelines-wrong-dr-mark-horowitz-tapering-off-antidepressants/
I was fortunate recently to interview Dr. Mark Horowitz. Dr. Horowitz is a training psychiatrist and researcher and recently co-authored, with Dr. David Taylor, a review of antidepressant withdrawal that was published in Lancet Psychiatry, which we’ve written about here at Mad in America (see here). Their article suggests that tapering off antidepressants over months or even years is more successful at preventing withdrawal symptoms than a quick discontinuation of two to four weeks.