Three weeks ago What would Batman do Now covered the issue of suicide in the military – an issue that had Batman missing in action, and the Joker suffering the adverse effects of psychotropic drugs. Then along came James Holmes to the premiere of Dark Knight Rises in Aurora. Most drugs that can cause suicide, including the antidepressants, mood-stabilizers, antipsychotics, … [Read more...] about The Hidden Gorilla
Archives for July 2012
One Script To Rule Them All
So Long and Thanks for all the Fish portrayed doctors in a rather flattering light – the victims of a tragedy. They were portrayed as losing out in a Faustian bargain when they failed to realize the hazards in making all new drugs available on prescription only. The bargain offered them a chance to entrench themselves inescapably in healthcare as the only legal source of all … [Read more...] about One Script To Rule Them All
There’s Something About Mary
A paper looking at antidepressants and birth defects in Denmark has just appeared. Anyone can download it and read for themselves (Jimenez-Solem et al 2012). It's worth reading. The published data demonstrate an increased rate of major birth defects on SSRIs which fits what almost all other studies have found. But this study also finds that women who have stopped their SSRI … [Read more...] about There’s Something About Mary
Herding Women
Since 2005, Paroxetine, first marketed by GlaxoSmithKline as Seroxat/Paxil, has carried warnings of birth defect risks. These risks led to litigation in the US – but not elsewhere. In the first case that went to court in the US in 2009, the Kilker case, the lawyers for Lyam Kilker argued that, even before Paxil was launched, there was good laboratory evidence that the … [Read more...] about Herding Women
A New Epidemic: Antidepressants During Pregnancy
This post is by Dr Adam Urato, a Professor of Obstetrics & Gynecology at Tuft's University. Imagine for a moment that a virus started affecting about 5% of all pregnant women—200,000 US pregnancies per year. Imagine that it caused significant pregnancy complications--more than 10% of those infected with the virus would have miscarriage, up to 20% or more would have preterm … [Read more...] about A New Epidemic: Antidepressants During Pregnancy
What Would Batman Do Now?
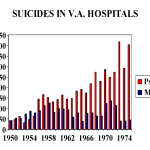
Johanna Ryan in her post Dependence Day points to serious problems linked to psychotropic drug use in the military and what seem to be recent alarming developments, but there is a 60 year history here. In the 1950s, the VA hospital system commissioned Norman Farberow to look at rising rates of suicides among veterans. He studied veterans hospitalized for either medical or … [Read more...] about What Would Batman Do Now?
Dependence Day
Author: Johanna Ryan, Labor Activist with Illinois Workers Compensation Lawyers (Chicago) Last month I watched as forty Iraq and Afghanistan vets led an antiwar march to the gates of the NATO summit in Chicago, and handed back their medals. At the rally, they described the toll the wars had taken on the troops as well as the people of Iraq and Afghanistan, and demanded their … [Read more...] about Dependence Day